Assessment of the risk to consumers as a result of disruption to the cold chain during direct supply of Qurbani meat and offal - full report
A risk assessment on allowing meat and offal to be provided to consumers without the normal chilling process during Qurbani.
Executive Summary
Qurbani is a religious practice involving animal slaughter that takes place during Eid al-Adha. Consumers who undertake their Qurbani in the UK wish to collect their meat and red offal as soon as possible following slaughter, which means these will not necessarily comply with chilling requirements set out in retained Regulation (EC) 853/2004. The supply of meat above 7 °C and offal above 3 °C may allow for the growth of pathogens, increasing the risk of illness. The pathogens that were chosen for inclusion in this assessment are non-typhoidal Salmonella enterica, Shiga toxin-producing Escherichia coli, and Clostridium perfringens. Their growth characteristics and prevalence in beef, lamb and goat meat and offal are discussed.
This risk assessment also considers three surveys carried out in the summer of 2021, targeting food business operators, official veterinarians and consumers. These surveys collected information on the origin of animals for Qurbani, quality assurance at the slaughterhouse, the chilling achieved post-slaughter, the route to consumers (either via a butcher or wholesaler, or consumers collecting their Qurbani directly), and consumer storage and cooking behaviours.
The assessment concluded that, given the number of factors affecting the risk to consumers from the supply of meat and offal for Qurbani, there were two important scenarios with distinct outcomes. In the typical scenario, which is the most likely outcome based on the collected data, there is no significant difference in risk to consumer health, and the risk level was established as Very Low (“very rare, but cannot be excluded”). In a reasonably foreseeable worst-case scenario, Salmonella spp. and STEC levels may increase by 1-2 log10 CFU/g, presenting an increased risk to the consumer. This risk level was established as Low (“rare but does occur”).
Significant uncertainties remain, including the temperature of the carcase and offal when it reaches consumers, epidemiological data linking cases of illness to the consumption of Qurbani meat and offal, and the prevalence and enumeration levels of the three pathogens in meat, especially goat, and offal. The overall uncertainty level for this assessment is High.
Lay summary
Qurbani is a religious practice that takes place during Eid al-Adha. Consumers practicing Qurbani typically wish to collect meat and red offal within a short time after slaughter, which means these products cannot complete normal chilling processes before leaving the slaughterhouse. This could permit greater growth of pathogens and has the potential to increase the risk of consumer illness. The FSA is working with industry and stakeholder groups to ensure that the risk to consumers under these conditions remains at an acceptable level. To help inform these discussions, the FSA commissioned this assessment to understand the difference in risk from allowing meat and offal to be provided to consumers without the normal chilling process.
Using the scientific literature, expert opinion and business and consumer survey data, we have assessed the effect of reported behaviours during the supply of Qurbani meat. Given the reported variation in the process, we chose to assess the difference in risk under both typical and worst-case scenarios. Differences between these scenarios included the temperature of the carcase at the time of collection, whether meat was collected directly by consumers or was collected by butchers in refrigerated vehicles, and whether the meat was thoroughly cooked before consumption.
We concluded that in a typical scenario the risk to consumers is Very Low (“very rare, but cannot be excluded”). However, in a worst-case scenario there is an increased Low level of risk (“rare but does occur”). We also identified several areas where more evidence would be helpful, and as a result identified a High level of uncertainty in our conclusion.
Glossary
| Term | Definition |
|---|---|
| FBO | Food business operator |
| IN category | Improvement Necessary category |
| MHI | Meat Hygiene Inspector |
| OV | Official veterinarian |
| Spp. | Species |
| STEC | Shiga toxin-producing Escherichia coli |
| UIN category | Urgent Improvement Necessary category |
1. Statement of purpose
1.1 Risk question
The risk question for consideration in this assessment is as follows:
Is there a significant (qualitative) difference in the microbiological health risk to the final consumer associated with the supply and consumption of bovine, ovine or caprine carcase meat and offal that has not been chilled to at least a surface temperature of 7°C (for meat) and a core temperature of 3°C for offal or below, prior to leaving the abattoir, compared to such carcase meat or offal that has been chilled to at least a surface temperature of 7°C (meat) and a core temperature of 3°C (offal) or below, prior to leaving the abattoir where mitigations are applied?
1.2 In scope
Only bovine, ovine and caprine carcase meat and associated red offal (liver, heart, lungs and kidneys) supplied by slaughterhouses in the UK during the Qurbani period directly to the final consumer, or via butchers/wholesalers acting as agents for the final consumer, are within scope of this assessment.
Details of mitigations implemented by industry are available in Section 7.1 of the Appendix.
1.3 Out of scope
This does not apply to any meat or offal that will be placed on the open market.
Out of scope:
- Carcases, half carcases and quarters of bovine, ovine and caprine meat transported fully chilled in compliance with retained Regulation 853/2004.
- Carcases, half carcases and quarters of bovine, ovine and caprine transported partially chilled in line with retained Regulation 2017/1981.
- All other body parts aside from the carcase, liver, hearts, lungs and kidneys from the above species.
- Fully chilled offal from bovine, ovine and caprine in compliance with Regulation 853/2004.
- Any carcase or offal from other species
- Meat that has been further processed for example, minced
In addition, non-bacterial pathogens, such as Toxoplasma gondii and viruses, are considered out-of-scope. Temperature abuse (lack of chilling) does not affect the proliferation of these pathogens within or on meat compared to correct chilling. Freezing of meat, which results in the inactivation of Toxoplasma gondii cysts, is out of scope.
1.4 Regulatory requirements
The regulatory framework for meat hygiene in Section I, Chapter VII (storage and transport), Annex III of retained Regulation (EC) 853/2004 (as amended) sets out legal requirements for the chilling of meat and offal to a core temperature of 7°C and 3°C, respectively. This is referred to as ‘fully chilled’ in this risk assessment. Qurbani religious custom and practice does not align with this regulatory framework as the timelines of this festival mean that consumers expect to collect meat and offal prior to full chilling.
Retained Regulation (EU) 2017/1981 allows for the partial chilling of meat transported from business to business, for example, from a slaughterhouse to a butcher. It allows for a maximum surface temperature of 7 °C upon transport, but the carcase must be fully chilled before final delivery to the consumer. This only applies to carcase meat and not offal. This is referred to as ‘partially chilled’ in this risk assessment.
To meet religious requirements during the Qurbani period, slaughterhouses are allowed to supply meat that does not adhere to the above regulations as long as certain mitigations are followed (see 7.1). Otherwise, the same rules and requirements apply when slaughtering animals for Qurbani as for any type of halal slaughter (DEFRA, 2015).
1.5 Background
Eid al-Adha, also called the "Festival of the Sacrifice", is a 4-day religious Islamic holiday celebrated worldwide. The date of the celebration varies from year to year and can take place in any season. In 2021, the festival occurred in July, in 2022 it will commence at sundown on Saturday 9th July, and it will remain in summer and spring months until 2030. It honours the willingness of Ibrahim to sacrifice his son as an act of obedience to God's command. The practice of Qurbani is a ritual livestock animal sacrifice and takes place during Eid al-Adha. The animal is usually a domesticated sheep, cow or goat, and traditionally, its meat is divided into three parts. One share is given to charity, another is kept at home, and a third is given to relatives or friends. As shown in Figure 1, this risk assessment does not consider processing following distribution to friends/family/the needy.
Generally, Muslim consumers wish to collect their sacrifice as soon as possible following slaughter, which does not allow for all meat and offal to be chilled to refrigeration temperatures. Some consumers go directly to the slaughterhouse to collect their Qurbani meat and offal, and others go to butchers who collect Qurbani meat on their behalf. The greatest demand for Qurbani occurs on the first day of Eid al-Adha.
To better understand the nature of the supply chain, the process at the slaughterhouse, and the delivery of Qurbani meat and offal to consumers, three questionnaires were filled in by food business operators (FBOs) for example, slaughterhouses, all official veterinarians (OVs) and consumers in 2021. These responses are recorded in Annex 1, and specific results discussed throughout.
1.6 Population under consideration
1.6.1 Overview
The population under consideration is Muslim residents in the UK who purchase Qurbani from a UK slaughterhouse. This is estimated in Section 1.6.2. From the data available it is thought that between 25% - 50% of the total Muslim population, which is around 3.3 million people, perform Qurbani in the UK and the rest donate their Qurbani outside of the UK. Vulnerable groups (young children or >65) form 38% of the Muslim population, though this is likely to be an overestimate.
1.6.2 Total population participating in domestic Qurbani consumption
According to the Office for National Statistics, the population of Muslims in Great Britain in 2016 was estimated to be 3,307,518 or around 5%, with a breakdown provided in Table 1 (NISRA, 2011).
| Country | Population of Muslims | Total Population | % Muslims |
|---|---|---|---|
| England | 3,161,629 | 54,394,168 | 6 |
| Wales | 47,409 | 3,065,708 | 2 |
| Scotland | 98,480 | 5,275,047 | 2 |
| Northern Ireland* | 3,832 | 1,810,863 | <1 |
There are limited data available on how many Muslims will consume Qurbani meat or offal in England and Wales and the number of servings (uncertainty). Information provided by a Senior Halal Sector Manager, following consultation with other stakeholders, reported that based on approximately 50,000 UK Qurbanis being performed each year, this would be consumed by approximately 900,000 people or 25% of the Muslim population (uncertainty) (Pers. comms., Stubbington, P., Dec 2021).
Responses from the 2021 consumer questionnaire show that out of 71 respondents, 28 (39%) reported undertaking their Qurbani in the UK. The remaining 43 (61%) reported performing Qurbani outside of the UK. This means that they paid to have an animal sacrificed for this purpose outside of the UK to donate to the needy and therefore did not obtain meat via a UK slaughterhouse. Taking consumer responses from the 2021 survey into account and the views of a Senior Halal Sector Manager (Pers. Comms. Stubbington, P., Dec 2021) it is suggested that between 50% - 75% of the Muslim population perform Qurbani outside the UK (uncertainty).
As of 2021, only abattoirs in England and Wales provide Qurbani meat and offal. There is little or no demand for Qurbani meat and offal in Scotland and Northern Ireland, however, this may change in the future.
1.6.3 Proportion consuming offal
There are limited data on how many people consume offal during the Qurbani period. 11 out of 28 respondents (39%) who performed Qurbani in the UK stated they received offal and the remainder did not. A further breakdown of the type of offal received is unknown. The Scholar’s opinion (Islamic Scholars are Muslims trained in Islam and Islamic law) also states that consumer expectations are for the carcase more than the offal (AHBD 2021 EID11 Scholars opinion).
1.6.4 At-risk groups
Data from Office for National Statistics, 2011, on the population of Muslims in England and Wales by age group are presented in Table 2. Data for Scotland and Northern Ireland are not reported. According to this data, vulnerable groups (young children and >65) account for 38% of the Muslim population. Young children are those aged 0-15, and as there is no further breakdown of ages within the data, this is likely to be an overestimation of the vulnerable population.
Table 2: Population of Muslims by age group in England and Wales in 2011. Data obtained from the 2011 census.
| Age (years) | Population of Muslims | % of total Muslim population |
|---|---|---|
| All categories | 2,706,06 | 100 |
| 0-15 | 895,137 | 33 |
| 16-24 | 414,245 | 15 |
| 25-34 | 543,783 | 20 |
| 35-49 | 526,286 | 19 |
| 50-64 | 219,789 | 8 |
| 65-74 | 67,199 | 3 |
| 75 and over | 39,627 | 2 |
2. Hazard identification
2.1 Microorganisms of concern
Criteria for inclusion of pathogens in this risk assessment are – bacterial pathogens that are likely to be found in raw beef, lamb or goat, and with cases or outbreaks linked to these raw meats within the UK or EU.
An EFSA opinion document (EFSA 2014) found that Salmonella spp., Shiga toxin-producing Escherichia coli (STEC), Listeria monocytogenes and Yersinia enterocolitica are the pathogens of greatest microbial relevance when considering chilling protocols for beef, pork or lamb carcases. Given its association with outbreaks caused by meat, Clostridium perfringens was also considered (Dolan et al, 2015.; Gormley et al., 2011). Discussion of whether each of these pathogens meets the criteria for inclusion is provided below.
2.1.1 Listeria monocytogenes
Listeria monocytogenes is a zoonotic, Gram-positive, rod-shaped bacterium. Listeriosis is very frequently associated with the consumption of chilled ready-to-eat foods such as pre-packed sandwiches, soft cheese, other dairy products, salad, smoked fish, and sliced cooked or cured meats, rather than raw bovine, ovine or caprine meat (Cartwright et al., 2013; Desai et al., 2019; EFSA, 2018), due to its widespread presence in the environment and persistence in the food processing environment (Bucur et al., 2018).
Listeria spp. can be present in animals. The 2019 EFSA One Health report shows that 1.4% of animals tested were positive for Listeria spp. and 27.2% of these positives were reported as being L. monocytogenes. The animals tested mainly consisted of cattle (82%), sheep (11%) and pigs (3%) but species-specific results were not reported. Other food-producing, wild, zoo and pet animals were also included in the figures.
The 2019 EFSA One Health Report does not appear to attribute any human cases of listeriosis to non-ready-to-eat bovine, ovine or caprine meat and cases reportedly linked to food-borne outbreaks appear linked to ready-to-eat foods.
2.1.2 Yersinia enterocolitica
Yersinia enterocolitica are zoonotic, Gram-negative coccobacilli. Y. enterocolitica cases are mostly thought to be related to the consumption of undercooked pork, or cross contamination of ready-to-eat foods from raw pork, as pigs are the main food animal reservoir for this pathogen (Fredriksson-Ahomaa et al., 2006; Rahman et al., 2011; EFSA 2014).
The 2019 EFSA One Health Report stated that 10% of non-ready-to-eat fresh meat from bovine animals tested positive for Y. enterocolitica. This represented 1 sample out of 10, reported by 1 EU member state. The report also showed that 0.8% of ‘domestic livestock animals other than pigs’, which included cattle, goats and sheep, as well as alpacas, fowl, reindeer and domestic solipeds, tested positive for Y. enterocolitica. This represents 145 samples out of 18,061 reported by 5 member states and 1 non-member state. (EFSA and ECDC, 2021).
From the EU zoonoses surveillance report, no cases of Y. enterocolitica appear to have been linked to bovine, ovine or caprine meat in 2018 and the one outbreak occurring that year was linked to pig meat and products thereof (EFSA and ECDC, 2019) which are outside the scope of this assessment.
2.1.3 Salmonella enterica spp.
Salmonella enterica non-typhoidal serovars, such as Enteritidis and Typhimurium, are Gram-negative bacteria commonly associated with foodborne illness. Transmission of Salmonella occurs via the faecal-oral route and the pathogen has a broad host range, including ruminants.
Recent EU data relating to outbreaks, taken from the 2018 EU Zoonoses report showed that out of a total of 296 Salmonella outbreaks across the EU in 2018, 3 were caused by bovine meat and products thereof, 3 were caused by sheep meat and products thereof and 3 were caused by other red meat and products thereof but this is not further broken down into animal species or ready-to-eat/raw products (EFSA and ECDC, 2019). All of these represented 1% of Salmonella outbreaks each in the EU in 2018. No outbreaks were identified as being caused by goat meat specifically.
The 2019 EU Zoonoses reported that 3 out of 926 Salmonella outbreaks were attributed to bovine meat and products thereof, 1 from sheep meat and products thereof, and 17 from mixed or other red meat (EFSA and ECDC, 2021).
According to recent Salmonella surveillance data there were 8,398 laboratory reports of cases of Salmonella in England and Wales in 2019. A recent Salmonella outbreak in the UK has been associated with consumption of lamb and mutton, with almost 300 cases reported in 2017 and 2018 (ESCAIDE 2021; APHA 2018). One outbreak with 62 cases was associated with lamb in 2019 (UKHSA, 2010).
2.1.4 Shiga toxin-producing E. coli (STEC)
Shiga toxin-producing Escherichia coli (STEC) are a group of E. coli characterised by their ability to produce Shiga toxins and cause gastrointestinal illness. The main reservoir for STEC (notably STEC strain O157) is believed to be ruminants, with transmission via the faecal oral route.
Within the EU, the food group most associated with STEC outbreak between 2010-2017 was bovine meat and products thereof, leading to 17 out of the 54 outbreaks (EFSA and ECDC, 2019). One outbreak in Norway in 2006 was attributed to the use of STEC contaminated sheep meat in dry cured sausages (EFSA, 2013). The 2019 EU Zoonoses reported that 4 out of 42 STEC outbreaks were attributed to bovine meat and products thereof and 1 from sheep meat and products thereof (EFSA and ECDC, 2021). Cross-contamination from raw meat to ready-to-eat foods has also been shown to be a pathway for transmission of STEC (Wilson et al., 2018).
According to the most recent PHE STEC surveillance data, there were 1,553 confirmed cases of STEC (607 O157 and 612 non-O157) in England and Wales in 2018. Between 2017-2019, there were 2 STEC outbreaks in the UK associated with bovine meat or products thereof, leading to 29 cases (EFSA 2017; EFSA 2019).
2.1.5 Clostridium perfringens
Clostridium perfringens is a Gram-positive, anaerobic, spore-forming, rod-shaped bacterium. It is found ubiquitously in soil and in the intestines of warm-blooded animals, including humans. Spores are metabolically dormant (they do not replicate) and extremely resistant to environmental stresses, such as heat. C. perfringens food poisoning commonly occurs when meat, poultry products or other cooked foods are undercooked or kept warm for prolonged periods, at temperatures of 12 °C – 60 °C, allowing the spores to germinate, forming vegetative cells that then rapidly multiply in the food.
Heat treatment of spores at 60 °C – 80 °C is generally required for activation of C. perfringens spores (de Jong et al., 2004; Duncan and Strong, 1968; Roberts, 1968). Without heat shock, only 3% of C. perfringens spores germinated in raw beef held at temperatures of 15 °C – 37 °C (Barnes et al., 1963). Although C. perfringens spores are the main concern in food products, vegetative cells may occasionally cause health problems by cross-contaminating ready-to-eat foods.
90 cases, with an 8% hospitalisation rate, were associated with 4 C. perfringens outbreaks in 2020 in the UK (DEFRA, 2021). Beef products were the most commonly reported vehicle in C. perfringens outbreaks (31% of C. perfringens outbreaks with 267 associated cases) between 2015 – 2020 in the UK. 50% of outbreaks due to lamb meat or products were caused by C. perfringens in that same period (DEFRA, 2021).
2.1.6 Summary
Given the low frequency of detection of Y. enterocolitica and L. monocytogenes in bovine, ovine and caprine animals and the limited evidence of human illness from these organisms as a result of consuming these meats, Y. enterocolitica and L. monocytogenes have been considered an unlikely cause of concern for this risk assessment. This risk assessment therefore concentrates on Salmonella spp., STEC and C. perfringens as the hazards.
2.2 Previous outbreaks associated with Qurbani meat
It is challenging to link cases/outbreaks to the timing of Eid al-Adha. Information is not routinely collected on religious status of human cases of Salmonella, C. perfringens or STEC, or if cases had consumed Qurbani meat or offal, making detection of these cases difficult to determine against normal seasonal variability and noise (uncertainty).
No information was available relating specific cases or outbreaks in the UK to Qurbani meat or offal, other than a cluster of Salmonella Typhimurium cases in Cardiff in 2021 (Whitworth, 2021). This consisted of a localised incident linked to the consumption of raw or lightly cooked red offal at a private event. Cooked lamb was also consumed. Two slaughterhouses provided the meat and offal consumed at the event and an OV inspection of one of these identified issues with hygiene practices and that offal was despatched at temperatures over the legal limit.
A literature search was carried out in PubMed and identified three potentially relevant papers describing foodborne outbreaks potentially associated with Eid al-Adha (methods provided in 7.2). Upon further examination, two of these were concerned with parasites such as Toxoplasma gondii, Echinococcus granulosus and Taenia spp., which are not considered relevant for this risk assessment as they do not multiply in raw meat. The final paper consisted of a report on the mass gathering for Eid al-Adha in Aqaba, Jordan, in 2010 where 30,000 to 70,000 visitors were expected, and this paper did not report any food poisoning outbreaks (Abdullah et al., 2013). This paper did not consider the potential limitations of the study which include underreporting of foodborne illness, particularly those that are self-limiting, and traceability difficulties of attendees who travelled to the event and returned home prior to illness.
The academic literature search found no papers describing outbreaks of foodborne disease in the UK with an epidemiological link to Eid al-Adha.
3. Exposure assessment
3.1 Growth of pathogens on bovine, ovine, and caprine meat and offal
Raw meat and offal typically have a high water activity, and a slightly acidic to neutral pH of 5 to 7, which is conducive for microbial growth (McPhail et al 2005). The exact conditions encountered in the cuts of meat and offal of the different species butchered for Qurbani is unknown (uncertainty).
3.1.1 Growth of Salmonella
Salmonella can grow at temperatures ranging from 7 °C - 44.6 °C, with an optimum growth temperature of around 37 °C (Tomkin et al 2015). Under laboratory growth conditions in broth medium, Salmonella will increase ten-fold in 24 hours when grown at 15.6 °C, and in 9 hours when grown at 21.1°C (Tomkin et al 2015).
A few studies have investigated Salmonella growth on meat tissue. In one study, where Salmonella was inoculated on beef; Salmonella levels doubled in 8.1 hours at 10 °C, in 5.2 hours at 12.5 °C and in 2.9 hours at 15 °C (Mackey et al., 1980). Another study investigated growth at 25 °C; Salmonella levels exhibited a 4-8 log10 increase in 24 hours, dependent on the pH and fat content of the beef (Grau, 1983).
No data were available from a literature search on microbial growth in bovine/caprine/ovine offal held at room temperature. Experiments on simulated temperature abuse of pork livers and kidneys showed that aerobic plate counts of fresh livers after holding at 30 °C for 6 or 12 hours increased by 1.07 and 2.99 log10 per cm2, those for fresh kidneys by 1.38 and 3.08 log10 per cm2, respectively (Hanna et al., 1982).
Growth of Salmonella spp. was simulated in Combase (Baranyi and Tamplin, 2004) and depends greatly on the temperature being modelled (see Table 3 for simulated growth). It should be noted that Combase predications generally overestimate bacterial growth as factors other than those included in the Combase model will generally limit growth behaviour.
Table 3: Simulated log10 growth of Salmonella spp. at various time-temperature combinations. Predictions were made using Combase, with pH set to 6, a water activity of 0.99 and other parameters set as default (Baranyi and Tamplin, 2004).
| Temperature (°C) | Time: 1 hour | Time: 2 hours | Time: 4 hours |
|---|---|---|---|
| 10 | 0.00 | 0.00 | 0.00 |
| 15 | 0.00 | 0.01 | 0.02 |
| 20 | 0.01 | 0.03 | 0.09 |
| 25 | 0.02 | 0.08 | 0.42 |
| 30 | 0.05 | 0.22 | 1.16 |
| 35 | 0.07 | 0.37 | 1.71 |
Based on the simulated and reported growth, time-temperatures combinations of 30 °C for 4 hours, 35 °C for 4 hours, or equivalent, are likely to significantly increase Salmonella levels.
3.1.2 Salmonella dose-response information
The infectious dose of Salmonella is generally high, although this varies between serovars, individuals and food vehicles (Kothary and Babu, 2001). A dose-response model fitted to data from 20 outbreaks, involving several food vehicles, gave an estimated ID50 the pathogen dose likely to cause illness in 50% of test subjects) of approximately 104 cells (World Health Organization and Nations, 2002). High fat foods consumed by vulnerable groups could have an infectious dose as low as 10-100 cells (for instance, consumed dose was estimated to be around 50 cells in a peanut sauce outbreak - World Health Organization and Nations, 2002). An infectious dose of 2.4 x 105 cells was calculated to be responsible for an outbreak of S. Enteritidis from roasted beef at a restaurant, which led to 3 illnesses (World Health Organization and Nations, 2002). Dose-response modelling based on data obtained from outbreaks indicates the risk of infection and illness increases as the dose increases (Glynn and Bradley, 1992; Teunis et al., 2010).
3.1.3 Growth of STEC
STEC growth has been observed in the range of 7 °C – 50 °C, although growth has also been reported in some strains at temperatures as low as 4 °C. It can survive freezing for extended periods. The optimal pH for growth is near-neutral, but growth has been reported at pH 4.4 and in some cases at pH 3.6. STEC also survives fermentation and drying process (for example, used in the manufacture of dry fermented meat). The minimum water activity for growth is 0.95.
Under laboratory growth conditions, STEC will increase ten-fold in 21 hours when grown at 15.6 °C and in 9 hours when grown at 21.1 °C (Tomkin et al 2015). When an E. coli strain isolated from sheep faeces was grown at 25 °C on beef muscle tissue, E. coli populations increased by between 4 and 8 log10 in 24 hours, dependent on the pH and fat content of the meat (Grau, 1983). It is not known if STEC strains would behave in similar manner (uncertainty).
Simulated growth of STEC depends greatly on the temperature being modelled (see Table 4 for simulated growth in Combase).
Table 4: Simulated log10 growth of E. coli at various time-temperature combinations. Predictions were made using Combase, with pH set to 6, a water activity of 0.99 and other parameters set as default (Baranyi and Tamplin, 2004).
| Temperature (°C) | Time: 1 hour | Time: 2 hours | Time: 4 hours |
|---|---|---|---|
| 10 | 0.00 | 0.00 | 0.00 |
| 15 | 0.00 | 0.01 | 0.02 |
| 20 | 0.01 | 0.02 | 0.07 |
| 25 | 0.02 | 0.06 | 0.25 |
| 30 | 0.03 | 0.12 | 0.6 |
| 35 | 0.04 | 0.15 | 0.78 |
Based on the simulated and reported growth, time-temperatures combinations of 30 °C for 4 hours, 35 °C for 4 hours, or equivalent, are likely to significantly increase STEC levels.
3.1.4 STEC dose-response information
The infectious dose for STEC is relatively low, although there is uncertainty particularly for strains other than the O157:H7 serovar. It is thought that exposure to fewer than 100 cells of STEC O157:H7 can cause infection. Exposure estimates have been reported from outbreaks where the concentration of STEC O157:H7 in the food at consumption could be determined; this was less than 700 cells in beef patties (WHO, 2018). Dose-response modelling based on data obtained from outbreaks indicates the risk of infection and illness increases as the dose increases (Phetxumphou, 2016).
3.1.5 Growth of Clostridium perfringens
C. perfringens vegetative cells are capable of rapid cell division. The maximum growth rate is dependent on the genetics of the strain, particularly the plasmid or chromosomal presence of the C. perfringens enterotoxin (Li and McClane, 2006). The optimal temperature range for growth is 37 °C – 45 °C (García and Heredia, 2011), though some strains can grow between 6 °C – 50 °C, most strains cease division at 15 °C or below and remain dormant until a return to favourable conditions (Taormina and Dorsa, 2004). Slow growth of vegetative cells has been observed at 20 °C, and rapid growth at 37 °C, but germination of spores was not observed at either of these temperatures without heat activation (Barnes et al 2008).
When grown under optimal laboratory conditions, some C. perfringens strains have a doubling time of seven minutes, with many strains capable of growing faster when inoculated onto beef than in thioglycolate broth at 41 °C (Willardsen et al 1978). Due to this rapid growth, C. perfringens spores remain a risk within the food chain even after cooking has killed vegetative cells. Cooking temperatures activate the spores, and once the temperature has reduced to <50 °C, spores germinate, rapidly dividing and potentially producing harmful toxins (Talukdar et al., 2016). As such, proper temperature control is vital in minimising the growth of C. perfringens, with cooling from 54 °C to 4 °C in < 9 hours resulting in less than a 1-log10 growth in CFU/g (Smith and Schaffner, 2004). Cooling from 54 °C to 4 °C over 12 hours leads to a 1.99-log10 increase, and cooling over 15 hours leads to a 3.73-log10 increase, with most of the growth occurring when the ground beef is at 54 °C to 28 °C.
Simulated growth of C. perfringens depends greatly on the temperature being modelled (see Table 5 for simulated growth in Combase).
Table 5: Simulated log10 growth of vegetative C. perfringens at various time-temperature combinations. Predictions were made using Combase, with pH set to 6, a water activity of 0.99 and other parameters set as default (Baranyi and Tamplin, 2004).
| Temperature (°C) | Time: 1 hour | Time: 2 hours | Time: 4 hours |
|---|---|---|---|
| 10 | 0.00 | 0.00 | 0.00 |
| 15 | 0.00 | 0.00 | 0.00 |
| 20 | 0.00 | 0.00 | 0.00 |
| 25 | 0.00 | 0.00 | 0.00 |
| 30 | 0.00 | 0.00 | 0.03 |
| 35 | 0.00 | 0.01 | 0.23 |
Based on the simulated and reported growth, the temperatures and times under consideration are unlikely to significantly increase C. perfringens levels.
3.1.6 C. perfringens dose-response information
The infectious dose for C. perfringens food poisoning is relatively high. Foodborne illness occurs when food becomes contaminated with large numbers of vegetative bacterial cells (>106 CFU/g) that carry the C. perfringens enterotoxin gene (García and Heredia, 2011). From reported and investigated outbreaks, approximately 108 vegetative cells per serving are necessary to cause diarrhoea (The EFSA Journal, 2005). A dose-response relationship modelled by Golden et al., 2009 from four C. perfringens human feeding studies gave an average ID50 (the pathogen dose likely to cause illness in 50% of test subjects) of approximately 1010 cells.
3.2 Food pathways
There are two overarching risk pathways for the supply of Qurbani meat and offal to consumers during the Eid al-Adha:
A. Meat / offal is collected from the slaughterhouse by a butcher / wholesaler on behalf of the consumer
B. Meat / offal is collected directly from the slaughterhouse by the consumer
Each of these pathways can apply to meat and/or offal from the slaughter of sheep, cattle or goats that have been supplied from either a small- or large-scale farm / producer or supplied directly by the consumer, for example if animals are home reared.
There are six key steps in the supply chain for Qurbani meat / offal that may affect the presence or growth of Salmonella, STEC and C. perfringens. These steps are illustrated in Figure 1 and discussed in turn in the following sections.
In the 2021 questionnaire, 38 out of 109 (35%) of OVs that responded to the questionnaire said that the FBO they worked with supplied Qurbani meat. Therefore, 38 FBOs are estimated to be suppling Qurbani meat in the UK. 20 out of 26; 77% of FBOs responded that they supplied Qurbani meat. 28 out of 71; 39% of consumers responded that they received Qurbani in the UK. These FBOs, OVs and consumers were then asked follow-on questions, which are discussed in the next sections.
It is noted that the respondents of the FBO and consumer questionnaires represent a smaller sample size, so the level of uncertainty associated with the responses is high. These data are self-reported, and therefore may be prone to bias or error (uncertainty).
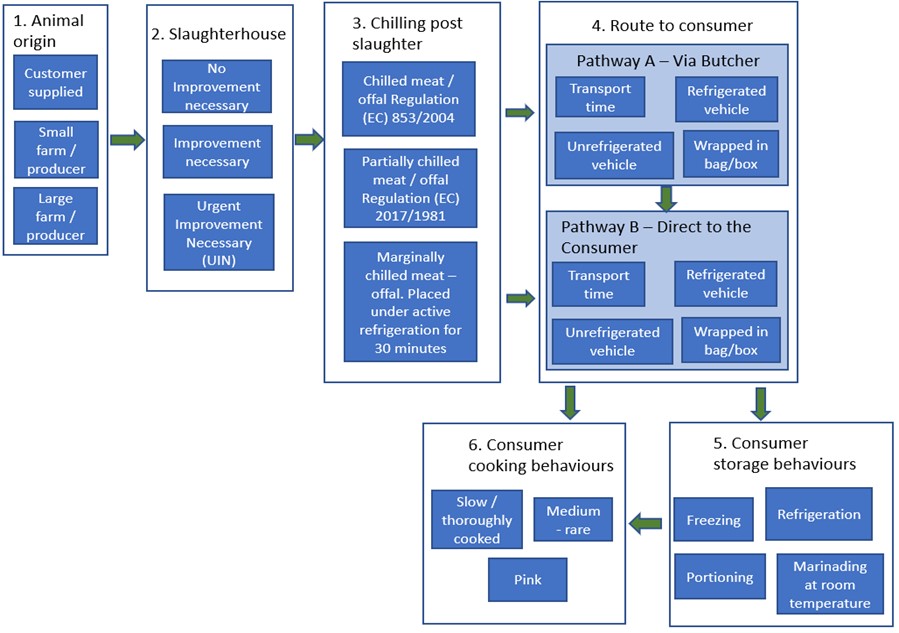
Figure 1: Risk pathways for the supply of Qurbani meat / offal from animal source to consumer showing factors considered in this assessment. This risk assessment does not consider further processing after consumer storage and cooking, or processing following distribution to friends/family/the needy.
3.3 Animal origin (Step 1)
3.3.1 Overview
In 2021, 32 FBOs were given a questionnaire to complete about the source of meat for Qurbani. Out of 20 respondents supplying Qurbani red meat throughout the Qurbani period, 2 (10%) stated the animals were sourced by customers (although farm origin information would be provided at slaughter, this information was not provided in the questionnaire),15 (75%) sourced animals from farms and livestock markets and 3 (15%) provided unclear answers. It is unknown if any of the animals sourced were imported before being purchased in GB, but this is considered very unlikely as animals are rarely imported for slaughter and many FBOs responded in the questionnaire that they sourced the animals locally.
Animals reared at home (for example, not at premises with the primary purpose of rearing animals for commercial purposes) for slaughter may have an increased likelihood of having acquired zoonotic pathogens, as health management practices may be reduced in comparison to those on small- and large-scale farms (uncertainty). However, it is likely there are far fewer animals on site, reducing the likelihood of pathogen transmission between animals, making the net effect uncertain (uncertainty).
All animals that are presented for slaughter must be accompanied by a food chain information form (FSA, 2020). This contains the individual or batch animal identification, confirms that the animals show no sign of disease and are not under any restrictions or withdrawal periods for medication. This does not mean they are free from zoonotic pathogens though, as animals, including sheep, goats and cows can carry these asymptomatically.
There is no evidence to suggest that the origins of animals will significantly affect pathogen growth in Qurbani meat and offal.
3.3.2 Consumer-supplied
There is no evidence that consumers who supply their own animals for slaughter undertake regular testing for pathogens considered within the scope of this document. Pathogen testing is expensive and would usually only be undertaken under veterinary advice for diagnostic reasons, for example to determine when there is disease and the cause. It is accepted that animals are potentially carriers of pathogens even when the animals are healthy.
It is possible that animals that are home reared may have an increased likelihood of disease introduction and spread due to reasons such as inappropriate animal health management practices and owners not being part of traditional livestock communication networks, but no specific data were available (uncertainty).
3.3.3 Commercial farm/producer
Livestock farming in the UK is highly regulated and operates to some of the highest animal welfare standards globally (World Atlas, 2021). Farms undergo numerous inspections throughout the year to try to prevent outbreaks of animal disease (including zoonotic diseases), prevent environmental pollution, check farmers comply with regulations, provide advice at the request of farmers and investigate complaints (Farming inspections, Gov.uk, 2016).
Intensive farming may carry a higher likelihood of pathogen transmission, particularly if living conditions and hygiene of livestock are poor (uncertainty). Intensive farming can lead to excessive crowding and keeping livestock above their capacity is associated with poor hygiene which can lead to the spread of infection (Conserve Energy Future, 2021).
There is no formal definition for a small farm / producer vs a large farm / producer. A smaller producer may have less intensive farming, decreasing the possibility of transmission of zoonoses between livestock (uncertainty). It may also be possible that the reasons for increased likelihood of disease introduction in smallholdings, such as not implementing appropriate animal health management practices and not being part of traditional livestock communication networks could also apply for small farms / producers (uncertainty).
No evidence could be located to quantify the difference in risk for animals reared for non-commercial versus commercial purposes in the UK.
3.4 Slaughterhouse (Step 2)
3.4.1 Overview
Prevalence of Salmonella in raw meat was found to be relatively low. Evidence suggests prevalence in offal is higher. UK surveillance indicates that the prevalence of STEC in meat is low, although no studies are available on its prevalence in offal. Recent data on C. perfringens prevalence in bovine, ovine and caprine meat and offal are unavailable, although recent outbreaks indicate it is still contaminating meat in the UK.
Both the proportion of contaminated carcases and the level of contamination can potentially be increased during the process of slaughter and evisceration. This is likely to be effectively mitigated by the normal hygienic procedures in operation. However, there may be a higher probability of contamination of products from slaughterhouses that have been given “Urgent Improvement Necessary” or “Improvement Necessary” status at audit. Increased contamination combined with the higher potential for pathogen growth in meat that is not thoroughly chilled could interact and result in higher pathogen load.
There is no difference in the slaughter method used for Qurbani compared to other halal meat produced outside of the Qurbani period, and therefore there is no relative difference in risk as a result of the processing method.
Slaughterhouse throughput during the Qurbani period, particularly Day 1, is significantly increased, which may affect the implementation of hygienic practices.
3.4.2 Prevalence of pathogen contamination in meat
Most meat contamination comes from heavily colonised areas or parts of the animal, such as the skin (fleece) and the gastrointestinal tract. The types and quantity of contamination reflect the animal’s indigenous microflora and its environment (Kwaasi, 2003). Both skin and gastrointestinal tract are removed from the animal during the slaughtering process. Studies have shown that per gram, offal (red and green) is more likely to be heavily contaminated with human pathogens than red meat (Little et al., 2008).
Following hide/fleece removal the rib cage is opened using a knife or splitting saw (depending on the species). The green offal (stomach and intestines including the intestinal tract) is removed using a knife, followed by the red offal (heart, liver, lungs and kidneys) also known as the pluck. The pluck is placed on a hook for inspection by the Meat Hygiene Inspector (MHI). During this process the pluck may be cross contaminated by stomach contents and contents of the intestinal tract (Pers Comms., Williams, M. Nov 2021). Areas of visible contamination would be rejected by the MHI, however not all contamination is clearly visible.
3.4.2.1 Salmonella
EU data show that Salmonella contamination in non-ready-to-eat meats in general (inc. broiler, turkey, pig, bovine and ‘other’ meat) was 2.6% in 2020 (EFSA and ECDC, Dec 2021). Monitoring of animal carcases at the slaughterhouse (after dressing but before chilling) found Salmonella in 1.6% of bovine carcases, 0.45% of sheep carcases and 1.2% of goat carcases. For meat and meat products from bovine animals prepared for retail, 0.46% of the samples were positive for Salmonella (EFSA and ECDC, Dec 2021). The level of contaminated bovine meat has not varied much over recent years. Data from 2016-2019 showed an average of 0.34% contamination (EFSA and ECDC, Dec 2021). Ovine and caprine meat were not listed.
UK surveillance of the microbiological contamination of raw red meat on retail sale in 2007 tested 3,249 beef samples, of which 0.18% (n=6) tested positive for Salmonella spp. 1,056 lamb samples were also tested, none of which tested positive for Salmonella spp. (FSA, 2010).
Data on contamination levels of offal are limited. One UK study examined raw beef and lamb meat and offal (Little et al., 2008). Of 1,514 beef meat samples tested, 1.1% were contaminated with Salmonella. Of 49 beef offal samples tested (inc. liver, heart, kidney, oxtail and tripe), 6.1% of samples were contaminated with Salmonella. This suggests that beef offal is more likely to be contaminated than beef meat, however, this study does not further break down which type of beef offal was contaminated therefore the prevalence of contamination in red offal is unknown. The study also tested 744 lamb meat samples. 1.7% of these tested positive for Salmonella. Of 161 lamb offal samples (inc. liver, heart and kidney), 3.1% tested positive for Salmonella. No recent UK data were found on bovine or ovine offal contamination (uncertainty); however, it is accepted that offal is more likely to be contaminated than meat for reasons previously discussed in this section. These studies did not carry out enumeration, therefore it is not possible to state the range of contamination levels.
No studies were found that measured the level of Salmonella in UK caprine meat or red offal (uncertainty). However, it is assumed that levels may be similar to those found in ovine meat as farming of both species is similar.
3.4.2.2 STEC
EU data show that STEC in non-ready-to-eat meat and meat products was detected in 3.8% of samples (EFSA and ECDC Dec 2021). Monitoring found 1.5% of fresh bovine meat samples were positive for STEC while 11.4% of fresh ovine meat samples and 7.7% of fresh caprine meat samples were positive (EFSA and ECDC Dec 2021).
UK surveillance of the microbiological contamination of raw red meat on retail sale in 2007 tested 3,249 beef samples, out of which 0.33% (n=1) tested positive for STEC O157. 1,056 lamb samples were also tested, none of which tested positive for STEC O157 (FSA, 2010). These studies did not carry out enumeration, therefore it is not possible to state the range of contamination levels.
No studies were found that examined STEC O157 contamination of UK caprine meat (uncertainty).
No studies were found that measured the level of STEC in UK bovine, ovine or caprine red offal (uncertainty).
3.4.2.3 C. perfringens
Sampling for C. perfringens as part of routine zoonotic surveillance is not performed in the UK or the EU. This pathogen was included in the FSA’s “UK survey of microbiological contamination of raw red meat on retail sale”, which ran from 2006-2007. C. perfringens was found on 9.99% of the samples overall (15.01% of beef samples and 5.2% of lamb samples). Despite the high prevalence, none of the samples contained levels near the reported infectious dose of this organism (105-108 CFU/g) (The EFSA Journal, 2005; FSA, 2010).
Although more recent prevalence data are available from studies in South Korea (Im et al., 2016) and Pakistan (Khan et al., 2015), these were not considered in the risk assessment as they were not deemed relevant enough to the UK situation.
It should be noted that not all C. perfringens strains are capable of causing disease, and that the presence of the bacteria does not necessarily pose a foodborne disease risk (uncertainty).
3.4.3 Quality assurance
3.4.3.1 Audit status
Slaughterhouses undergo periodic audits carried out by OVs and may be assessed as “Improvement Necessary” (IN) or “Urgent Improvement Necessary” (UIN). Further information on how this classification is achieved is given in Section 7.3 of the Appendix.
From the OV responses provided in 2021, 9 slaughterhouses (28%) providing Qurbani meat had UIN or IN status and 23 (72%) did not. The proportion of slaughterhouses that fell into the UIN or IN categories across the UK in 2019 - 2021 was around 3% (Pers comms., Field Vet Lead, Jan 2022). The sections of the audit that require improvements are not known (uncertainty). There is the potential that slaughterhouses requiring improvement could be associated with greater cross contamination risks compared to those that do not, as multiple sections of the audit relate to hygienic practices (uncertainty).
3.4.3.2 Qurbani Operating Procedures
FBOs are advised to have Qurbani operating procedures for supply of Qurbani which list requirements of good practices such as requirements for a minimum chilling time of 30 minutes, collection of traceability information and the provision of customer leaflets (AHDB EID01 2021).
According to the 2021 OV questionnaire, 28 (80%) FBOs had Qurbani operating procedures in place for the supply of meat direct to final consumers, and 7 (20%) FBOs did not. Similarly, 29 (83%) FBOs had Qurbani operating procedures in place for the supply of meat to final consumers via a butcher/retailer/wholesaler acting as an agent, and 6 (17%) did not.
In 2021, 25 out of 35 (83%) OVs or Meat Hygiene Inspectors had the opportunity to carry out verification checks on the implementation of these Qurbani operating procedures, with 5 non-compliances observed.
The five non-compliances identified included:
- no/incomplete consumer declaration provided (2 FBOs)
- no consumer information provided (1 FBO)
- meat not wrapped before dispatch (1 FBO)
- meat not stored under active chilling before dispatch (1 FBO)
- meat stored under active chilling for less than 30 minutes (1 FBO).
In one case, the OV carried out informal enforcement.
3.4.4 Throughput during the Qurbani period
In the 2021 questionnaire, 20 FBOs were asked what their daily throughput of animals on Day 1 of the Qurbani period was in comparison to daily throughput outside of the Qurbani period. There were varying responses, although in most cases (16 out of 20; 80%), the throughput was larger on Day 1 of the Qurbani period. On average, the total throughput is doubled on Day 1 of the Qurbani period, compared to a regular day, which may impact hygiene practices (uncertainty).
3.4.5 Processing after slaughter
Information from Euro Quality Lambs states that Qurbani carcase is cut into 6 primal cuts – 2 shoulders, 2 loins and 2 legs and final cutting takes place at a butchers. It is unknown whether this is the same for other slaughterhouses (uncertainty). There is no evidence available to suggest that consumers or butchers collect meat from the slaughterhouse that has been processed in other ways such as mincing.
Following slaughter and processing there is the risk that slaughter areas or other environments such as storage areas and chillers may become contaminated by excreta and blood (uncertainty). This risk of contamination is likely to be effectively mitigated by the normal hygienic procedures in operation at abattoir facilities, such as those required under the Food Safety and Hygiene (England) Regulations 2013. These should include clean-down processes and access for workers to well positioned showering facilities which prevent cross-contamination of other areas of the facility.
The increased throughput of animals for slaughter and processing during the Qurbani period may lead to disregard for normal hygienic practices (uncertainty) and increased likelihood of cross-contamination.
3.5 Chilling post slaughter (Step 3)
3.5.1 Overview
Information gathered from the 2021 FBO questionnaire shows that the majority of carcase meat provided during Qurbani 2021 was supplied above regulatory limits (7°C) and that more carcases were supplied marginally chilled than fully chilled directly to consumers and via butchers.
From the information gathered during the 2021 FBO questionnaire on core and surface temperature achieved for offal, the majority of FBOs achieved a temperature of <3°C (as per Regulations (EU) 853/2004), however, a few reported selling offal at temperatures above the legislative limits. The quantity of offal sold above legislative limits is unknown (uncertainty).
There is an increased likelihood of pathogen growth (Salmonella, STEC, and C. perfringens) on Qurbani meat and offal that is only marginally chilled if the pathogen is present. The level of growth is difficult to estimate and data on levels of pathogens in unchilled Qurbani meat are unavailable (uncertainty). Offal is more likely to be contaminated than meat, as described in Section 3.4.2, increasing the risk associated with offal that is supplied above regulatory limits (3°C).
5.5.2 Implementation of regulatory requirements for chilling
In 2021, the regulatory requirement was for all offal from the slaughterhouses to be sold fully chilled, however, this was not always the case, as outlined below.
Of the 26 slaughterhouses, which, according to the OV questionnaire supplied offal to consumers via butchers/wholesalers acting as agents, 19 (73%) supplied offal that was chilled to 3°C or below (as per Regulations (EU) 853/2004), 3 (12%) supplied marginally chilled offal (above legislative limits), and 4 (15%) were unsure.
Most FBOs provided marginally chilled carcases, although some also provided fully chilled and partially chilled meat. Further details of these results are provided in Section 7.4 of the Appendix.
In the 2021 questionnaire, FBOs were asked to give an indication of the average carcase and offal temperature achieved prior to sale. Data obtained show a range of temperatures (see Table 6). It is unknown whether all carcases and offal from each FBO were at or around their stated temperature in the questionnaire.
Table 6: average temperature of Qurbani carcases and offal, as reported by FBOs in the 2021 questionnaire. Core temperature and surface temperature measurements are reported separately.
| Temperature (°C) | FBOs (n) Core: Carcase | FBOs (n) Core: Offal |
FBOs (n) Surface: Carcase |
FBOs (n) Surface: Offal |
|---|---|---|---|---|
| Temperature not recorded | 2 | 0 | 1 | 0 |
| ≤3°C | 0 | 7 | 0 | 8 |
| ≤7°C | 2 | 1 | 0 | 1 |
| ≤10°C | 1 | 0 | 1 | 0 |
| ≤15°C | 1 | 1 | 3 | 0 |
| ≤20°C | 0 | 0 | 3 | 0 |
| ≤25°C | 0 | 0 | 1 | 0 |
| ≤30°C | 1 | 0 | 1 | 0 |
| ≤35°C | 2 | 0 | 0 | 0 |
There is more likelihood of pathogen growth on meat and offal that is supplied above legislative limits. The extent to which the supply of unchilled meat occurs, outside of the results of the 2021 questionnaire, is unknown.
3.6 Route to consumer (Step 4)
3.6.1 Overview
Two potential routes were identified by which consumers may obtain their Qurbani meat or offal. The first is via a butcher or agent, who will collect the unchilled (uncertainty) carcases / offal on behalf of consumers and then chill and likely portion the meat (uncertainty) before providing it to the final consumer – Pathway A. The second route to consumer is the consumer directly procuring the carcase meat or offal from a slaughterhouse – Pathway B (see Figure 1). This may be in the form of whole or half carcases (uncertainty).
Qurbani meat that is transported unrefrigerated for longer journeys could be exposed to time and temperature combinations that allow for growth of the pathogens under consideration.
While 39% of consumers did report collecting their Qurbani in refrigerated storage such as a cool box or cool bag, it is uncertain how effective this was. The likelihood of pathogen growth is increased for pathway B (collection via consumers) for meat and offal distributed above legislative temperatures in comparison to pathway A because 25% of consumers collected Qurbani in refrigerated vehicles compared to 95% of butchers, according to FBOs.
In 2021 it was more common for butchers to collect meat / offal on behalf of the consumer, decreasing the chances of temperature abuse. Whether this will remain true for subsequent years is uncertain (uncertainty). It was estimated that about a quarter of carcases are collected directly by consumers and three quarters by butchers or agents on behalf of consumers (uncertainty). Offal is less commonly provided to consumers overall than carcase meat.
Pathogen levels achieved after transport would depend on the levels present after slaughter, but very low doses of STEC can cause illness. Very low levels of Salmonella can cause illness in some vulnerable populations. Given this, cross contamination of surfaces or other foods could potentially lead to infection from Qurbani meat that is not hygienically handled.
3.6.2 Via a butcher/agent
In 2021 most Qurbani meat and offal was supplied to the final consumer via a butcher or agent. This was supported by the findings of all three questionnaires, although the exact proportion of carcases supplied by both routes is difficult to estimate. In the consumer questionnaire, 22 of 28 (79%) of respondents said that a butcher or agent collected their Qurbani. Out of 36 respondents, OVs reported that 19 (52.8%) FBOs provided Qurbani to butchers/wholesalers only, 4 (11.1%) provided Qurbani directly to consumers only and 13 (36.1%) supplied both. FBOs also reported the number of carcases supplied to consumers and butchers/agents that were fully chilled or marginally chilled (Table 7).
Table 7: Average number of carcases reported by FBOs to be supplied to consumers directly and to butchers/agents.
| Type of Establishment | Number of fully chilled carcases | Number of sheep/lamb marginally chilled | Number of other species marginally chilled |
|---|---|---|---|
| Consumers | 424 | 687 | 9 |
| Butchers/agents | 1342 | 2025 | 35 |
Given these data, an estimated 25% of carcases are assumed to be collected directly by the consumer and 75% collected by a butcher or agent.
Where whole or part carcases are picked up, a butcher has the facility to butcher and pack the meat into portions, and refrigerate the meat, helping to reduce the likelihood of cross contamination in the home of the consumer.
In 2021 OVs were asked whether Qurbani offal was collected by a butcher/wholesaler from the slaughterhouse, 26 (74%) responded ‘yes’ and 9 (26%) responded ‘no’.
In 2021, FBOs were asked how Qurbani meat and offal were collected and transported when collected by a butcher/wholesaler:
- 19 out of 20 (95%) reported meat/offal was collected in a refrigerated vehicle and 1 (5%) did not answer.
- FBOs reported meat was wrapped in a bag most of the time (14 out of 20, 70%). 3 (15%) reported in a box, 2 (10%) reported in a bag and box and 1 (5%) did not respond.
- FBOs reported that butcher/agent journey length ranged from <30 minutes to >2 hours. The most common journey length was 30 minutes – 1 hour.
Meat collected in a refrigerated vehicle by a butcher is likely to undergo less temperature abuse than an unrefrigerated vehicle, however if the meat and offal is collected above legislative temperatures (uncertainty), the meat may still be above legislative temperatures following transit due to limitations of the vehicle chiller (uncertainty). Refrigerated vehicles will likely not chill meat as efficiently as blast chillers used in slaughterhouses. There is uncertainty regarding journey length and therefore the amount of time meat may remain above legislative temperatures (uncertainty) as the responses from the 2021 may not be representative of future years.
3.6.3 Direct to the consumer
Around a quarter of Qurbani meat is assumed to have been provided to consumers directly from the slaughterhouse. It is unknown whether families took their carcases to a local butcher for portioning (uncertainty). 12 out of 20 (60%) FBOs stated that they supplied no offal directly to consumers.
Information found on Euro Quality Lambs, a supplier of British lamb meat who slaughter on site, provides customers with information about how they should collect their Qurbani from the slaughterhouse and subsequently handle and cook their Qurbani hygienically. The FSA recommended the supply of health information and consumer advice for the direct supply during Qurbani 2021. 31 out of 36; 86% of OVs stated that slaughterhouses supplied customers with information leaflets.
In 2021 FBOs and consumers were asked how Qurbani meat and offal was collected and transported when collected directly by the consumer:
- 11 out of 28 (39%) consumers collected their Qurbani in refrigerated storage (cool box or cool bag) and 17 (61%) said it was not.
- Out of 20 FBOs 5 (25%) reported that consumers collected their Qurbani in refrigerated vehicles, 6 (30%) said consumers did not, 4 (20%) said on some occasions and 5 (25%) did not state.
- FBOs reported meat was wrapped in a bag most of the time (14 out of 20, 70%). 3 (15%) reported in a box, 2 (10%) reported in a bag and box and 1 (5%) did not respond.
- FBOs reported that consumer journey lengths ranged from <30 minutes to >2 hours. The most common journey length was 30 minutes – 1 hour. FBO knowledge of consumer travel times is uncertain.
- Most consumers reported travel times of < 1 hour (20 out of 27; 74%). Journey lengths of about 1 hour (1 consumer) and 2 hours (3 consumers) were also reported.
The temperature of the meat during transport is unknown (uncertainty). There is an increased likelihood of temperature abuse when meat and offal is collected in unrefrigerated vehicles and/or cool bags and boxes which are limited in their ability to maintain the chill chain, and may only, at best, maintain the temperature of the meat (uncertainty).
It is unknown how well protected the meat and offal is that was wrapped in a bag. The bag may not be airtight or leak proof. If the bag was not well sealed this could lead to increased risk of cross-contamination (uncertainty).
There is uncertainty regarding how far the Qurbani is transported and therefore the length of time the meat remains unchilled and at temperatures that may support microbiological growth. Given that the date of Eid al-Adha varies year by year the risk will also vary. Temperature abuse is more likely to occur during the warmer summer months, but it is also possible for consumers to have the heating on in their car during colder months (uncertainty).
There is increased likelihood of pathogen growth and cross-contamination if consumers collect meat in unrefrigerated vehicles, meat is not well wrapped, and journey lengths increase (uncertainty).
3.7 Consumer storage behaviours (Step 5)
3.7.1 Overview
Refrigeration and freezing will pause microbial growth, with 21 out of 28 (75%) consumers reporting that they refrigerate or freeze their Qurbani when they arrive home. Two out of 28 consumers (7%) reported leaving it at room temperature for marinading. The level of pathogens may increase if consumer hygiene practices are poor and meat is left marinading for hours at room temperature. There is a cross contamination risk between raw Qurbani meat and offal and ready-to-eat foods.
3.7.2 Storage practices
Consumers were asked what they do with their Qurbani meat when it arrives at home. Answers included a range and combination of activities such as portioning meat, storing in a fridge or freezer, storing at room temperature for marinading and cooking straight away. Most consumers (23 out of 27 responses; 85%) reported portioning meat at home, although further detail was unavailable due to the design of the questionnaire. For the purpose of this risk assessment, it is assumed that the carcase will have already been cut down into at least primal cuts by the slaughterhouse or butcher.
Consumers were asked what they did with any meat that wasn’t for distribution or cooking. 21 out of 28 (75%) respondents said they store it in a freezer, 3 (11%) did not have uncooked leftovers, 2 (7%) reported storing leftovers in a fridge, and 2 (7%) left it at room temperature for marinading (uncertainty).
Advice is given to customers collecting carcases above the legislative temperature to cook, refrigerate or freeze their meat as soon as possible. Most (27 out of 36 responses; 75%) OVs in a 2021 questionnaire said that customers signed customer declarations and most (31 out of 36 responses, 86%) said that customers were provided with information leaflets.
3.8 Consumer cooking behaviours (step 6)
3.8.1 Overview
Cooking is a vital step for significantly reducing the risk of illness from consuming meat and offal as a result of any bacterial contamination present. A majority of consumers slow cook / thoroughly cook Qurbani meat which is sufficient to eliminate any vegetative pathogens present. Medium-rare lamb meat is also unlikely to present a foodborne illness risk as contamination with the hazards identified is most likely to occur on the surface of meat which is more likely to reach the necessary temperatures. 70 °C for 2 minutes or equivalent is considered the necessary cooking temperature/time combination to sufficiently eliminate pathogens. There may be an increase in risk from the consumption of temperature-abused offal if this is cooked rare, however, most offal was supplied at regulatory temperatures (≤3°C) in 2021. It is unknown if this will continue to be the case in future years (uncertainty). Undercooked lamb and veal liver has been associated with foodborne outbreaks (Gaulin et al., 2018; Hess et al., 2008; Whitworth, 2021).
Cross-contamination of ready-to-eat foods and food contact surfaces may result in illnesses, but more evidence is needed to quantify this risk.
3.8.2 Cooking practices
Consumers were asked how their household cooked Qurbani meat. Of 27 respondents, 18 (67%) said ‘slow cooked/thoroughly cooked’, 1 (4%) said ‘medium-rare or pink in the middle (lamb chops, liver, etc)’, 8 (29%) said ‘slow cooked/thoroughly cooked and medium-rare or pink in the middle (lamb chops, liver, etc). This risk assessment considers 9 out of 27 consumers (33%) to cook their Qurbani medium-rare or pink in the middle.
Improper cooling following cooking is thought to be responsible for a majority of C. perfringens outbreaks (Dolan et al. 2015). Spores of C. perfringens are able to survive the cooking process and, during slow cooling (holding foods at 40 °C – 50 °C at buffets or other events) and unrefrigerated storage, germinate to form vegetative cells. This risk exists whether or not carcases and offal have reached the required temperatures in the legislation, and it would not be made significantly worse by the levels of chilling observed for Qurbani in 2021, as spores do not multiply under these conditions.
4. Hazard characterisation
4.1 Salmonella spp.
4.1.1 Background
Salmonella is a well-recognised food safety hazard which can cause infectious intestinal disease in humans via ingestion of contaminated food or drink. Any Salmonella serovar is considered to be potentially hazardous to health, particularly if food hygiene is poor and/or sufficient cooking is not undertaken prior to consumption.
Non-typhoidal serovars are commonly associated with foodborne infection. The major serovars in the UK are S. Enteritidis and S. Typhimurium although many other serovars are reported. Salmonella serovars have a broad host range across mammals including those relevant for this scoping document (cattle, sheep and goats).
4.1.2 Symptoms of illness
The symptoms of Salmonella infection can range from asymptomatic carriage to severe diarrhoea. The incubation period of non-typhoidal Salmonella infection is usually from 12 to 96 hours, although periods of 96 to 144 hours (4 to 6 days) are not unusual and incubations of 7 to 9 days and occasionally longer also occur (Eikmeier et al., 2018). The principal symptoms of mild fever, nausea and vomiting, abdominal pain and diarrhoea last for a few days but can persist for a week or more. Whilst the illness is usually self-limiting, it can be more severe in vulnerable groups, including the elderly, young and immunocompromised, and may lead to systemic infection or death. After symptoms have subsided, carriage and shedding of the organism can occur for a few weeks, up to a few months. This can lead to secondary cases of infection through either direct contact with shedding individuals or cross-contamination. A study of the burden from foodborne disease in the UK has assigned 0.21 quality adjusted life years loss per salmonellosis case (Daniel et al., 2018). Quality adjusted life years loss is an economic term combining the impact from both length of life and quality-of-life losses. One quality adjusted life year is equal to 1 year of life in perfect health.
4.2 Shiga toxin-producing E. coli
4.2.1 Background
Shiga toxin-producing E. coli (STEC) are a group of E. coli characterised by their ability to produce Shiga toxins (stx1 and stx2 or their variants), designated so because of their similarity to the toxin produced by Shigella dysenteriae.
Beef cattle are the main reservoirs of STEC although other ruminants also carry them (Zschöck et al., 2000). The pathogen can be present in ruminant faeces, hide and carcases and contaminate meat during slaughter and later processing stages. STEC will be present on the surface of the meat, and due to further processing, such as mincing, dicing and sausage-making, can end up throughout the final product. Transmission can also occur through direct or indirect contact with animals or their environments, and person to person spread via the faecal oral route.
4.2.2 Symptoms of illness
All STEC strains are potentially pathogenic in humans, capable of causing diarrhoea and all STEC subtypes may be associated with severe illness, for example, haemolytic uremic syndrome (HUS), bloody diarrhoea and/or hospitalisations. Asymptomatic carriage can also occur. HUS develops in approximately 10% of patients infected with STEC O157 and is the leading cause of acute renal failure in young children. The incubation period is generally 1 – 6 days. A study of the burden from foodborne disease in the UK has assigned 0.06 quality adjusted life years loss per STEC O157 case (Daniel et al., 2018).
4.3 C. Perfringens
4.3.1 Background
C. perfringens is a rapid-growing microorganism widely distributed in nature that can be found in soil, dust, and in the intestinal tract of humans and livestock. It is commonly found on raw meat and poultry and can also be found on the surface of vegetable products (Abdelrahim et al 2019, FSA, 2010). The ability of this microbe to form heat-resistant spores contributes to its survival and its prevalence as a foodborne pathogen. Not all C. perfringens strains are capable of causing disease, and the presence of the bacteria does not necessarily pose a foodborne disease risk (uncertainty). The virulence of C. perfringens is caused by the production of the enterotoxin following sporulation in the intestine.
4.3.2 Symptoms of illness
The symptoms of C. perfringens foodborne infection are typically mild and exhibit self-limiting acute diarrhoea with abdominal cramps, nausea and pain. The illness is usually self-limiting, and the symptoms are usually not serious enough to consult a physician, although they can be more severe in vulnerable groups, including the elderly, young and immunocompromised, leading to systemic infection and death. Illness generally lasts no more than 24 to 48 hours. The incubation period is typically between 8 to 24 hours.
Linking the cause of an outbreak to C. perfringens is difficult as healthy individuals can have high numbers of spores in their faeces and not all strains are able to produce enterotoxin (Brynestad and Granum, 2002). Given the mild illness caused by C. perfringens, there is significant underreporting associated with it – it caused an estimated 85,000 cases and 13,000 GP presentations in the UK in 2018 (Holland et al., 2020). It has a high under-ascertainment ratio, as testing is only done for the enterotoxin during outbreaks (Holland et al., 2020). A study of the burden from foodborne disease in the UK has assigned 0.004 quality adjusted life years loss per C. perfringens case, making it the least severe out of 14 foodborne pathogens (Daniel et al., 2018).
5. Risk characterisation
This assessment evaluates the risk from the supply and consumption of bovine, ovine or caprine carcase meat and offal that has not been chilled to at least a surface temperature of 7°C for meat and a core temperature of 3°C or below for offal prior to leaving the abattoir for the duration of Eid al-Adha, compared to such carcase meat or offal that has been chilled according to regulatory requirements.
Maintaining the chill chain is vital in the case of raw meat at retail, which is usually kept for several days before purchase by consumers. Consumers may then take a few hours to reach their home and store the meat in a refrigerator that is often above the recommended temperature of 0 – 5°C (Biglia et al., 2017; Evans and Redmond, 2016).
In the case of Qurbani meat, the meat is often purchased on the day of slaughter and consumed that day, therefore decreasing the opportunity for pathogen growth in the first instance. Demand for Qurbani meat and offal is limited to a period of four days a year. However, it is likely be subjected to other temperature abuses, particularly during transport.
5.1 The effect of risk mitigation strategies
Several risk mitigations strategies were put in place, as part of Qurbani operating procedures, for the 2021 Eid al-Adha festival. These included:
- partial chilling of meat before direct supply (meat to be placed under active refrigeration for at least 30 minutes before dispatch)
When compared to unchilled meat, the partial chilling of meat before direct supply decreases the surface temperature of the meat, which for whole cuts of meat is where the highest microbial load will be concentrated. This will reduce microbial growth compared to unchilled meat. There are limited data on what temperature will be achieved with partial chilling, and therefore extent of the effect on microbial growth (uncertainty). Both unchilled and partially chilled meat will support greater microbial growth when compared to meat chilled according to regulation.
- supply of health information and consumer advice on the cooking and handling of the Qurbani meat
Providing consumers with advice on safe handling and cooking of their Qurbani provides confidence that cross-contamination and risky behaviours are minimised. 86% of OVs reported consumers were provided with information leaflets. It is unknown if all consumers have access to advice.
- measures in place to minimise cross-contamination, including suitable wrapping
Suitable wrapping to minimise cross-contamination should be airtight and leak proof. It is unknown how often wrapping used by FBOs adheres to this guidance (uncertainty).
- provision of offal that has been chilled for 24 hours to consumers who accept it
Offal that has been placed in a chiller for 24 hours before being offered as Qurbani will present less risk of pathogen growth than unchilled offal.
- additional consumer information provided about the risks specific to offal and the Scholars opinion in relation to providing fully chilled offal from the previous day’s production
It is unknown if consumers are provided with additional information specifically related to offal. Offal is more likely to be contaminated at slaughter and have internal contamination, therefore advice specific to offal would provide reassurance that consumers were aware of the associated risk and reasons for the Scholars opinion.
Further mitigations that are being considered include:
- requiring slaughterhouses to have had satisfactory results for the two months prior to Qurbani, as determined by OVs
Consecutive satisfactory results provide greater confidence that slaughterhouses apply adequate hygiene practices.
- requiring the slaughterhouses to have been characterised as ‘no improvements necessary’ in their latest audit
Audit status of ‘no improvements necessary’ provides greater confidence that slaughterhouses are performing to a good standard including adequate hygiene practices compared with slaughterhouses with UIN or IN status.
5.2 Definition and justification of scenarios
Given the number of factors affecting the risk to consumers from consuming meat during the Qurbani period, the difference in risk between meat produced for Qurbani and fully chilled meat will depend on the scenario considered. To reflect this, we have assessed the risk under two distinct scenarios: a ‘typical’ scenario and a ‘reasonably foreseeable worst-case’ scenario.
5.2.1 Typical scenario
From the data gathered during the 2021 questionnaires, we consider a typical scenario to involve meat and offal collection in a refrigerated vehicle via a butcher at 15°C or below, and fully chilled respectively. Consumers will then store the meat and offal in a refrigerator / freezer or thoroughly cook / slow cook their Qurbani. The justification of risk for each step in the pathway for the typical scenario is shown below:
Step 1: Animal origin. At least 75% of FBOs sourced animals for Qurbani in the normal way (farms and livestock markets) meaning there is no difference in risk resulting from this step.
Step 2: Slaughterhouse. No significant concerns were identified following audit for a majority (72%) of slaughterhouses supplying meat during Qurbani which responded to the questionnaire.
Step 3: Chilling post slaughter. In 50% of cases, meat was distributed at 15°C or below. In 83% of cases offal was distributed fully chilled (3°C or below), indicating no significant difference in risk.
Step 4: Route to consumer. In an estimated 75% of cases, butchers collected meat and offal from the slaughterhouse (Pathway A). In 95% of these cases, butchers collected meat and offal in refrigerated vehicles indicating no significant concerns.
Step 5: Consumer storage behaviours. 75% of cases reported refrigerating or freezing their Qurbani. Storing meat and offal in this manner would limit any further microbial growth.
Step 6: Consumer cooking behaviours. 67% of cases reported slow cooking or thoroughly cooking their Qurbani. If meat and offal achieve a cooking temperature of 70°C for 2 minutes, this would eliminate any vegetative pathogens.
5.2.2 Worst-case scenario
From the data gathered during the 2021 questionnaires, we consider a reasonably foreseeable worst-case scenario to involve meat and offal collection in an unrefrigerated vehicle directly by consumer at 30°C and above, and 10°C and above respectively. Following a journey length of around 2 hours, consumers will then leave uncooked meat and offal at room temperature for marinading and cook their Qurbani medium-rare or pink in the middle. The justification of risk for each step in the pathway for the worst-case scenario is shown below:
Step 1: Animal origin. Although some animals may have come from smaller holdings, no evidence was located to indicate a different risk for these animals. No increase in risk is therefore assumed for this step.
Step 2: Slaughterhouse. Some slaughterhouses (28%) had urgent improvement necessary or improvement necessary status at audit, indicating major and/or critical non-compliances in areas which may represent a risk to public health. Evidence allowing this risk to be quantified was unavailable (uncertainty).
Step 3: Chilling post slaughter. In 22% of cases, meat was distributed at 30°C and above. In 6% of cases, offal was distributed at 10°C and above. Particularly for meat, this indicates a significant difference in risk as a result of increased likelihood of pathogen growth at this step of the risk pathway.
Step 4: Route to consumer. In an estimated 25% of cases, consumers collected meat and offal directly from the slaughterhouse (Pathway B) in unrefrigerated vehicles (75% of the time). The maximum journey length reported by 4% of consumers was around 2 hours. This indicates a significant difference in risk as a result of increased likelihood of pathogen growth and potential for cross-contamination as consumer hygiene practices are unknown.
Step 5: Consumer storage behaviours. In 7% of cases, consumers left uncooked meat at room temperature for marinading. Marinading time was not stated (uncertainty). This indicates a significant difference in risk as the exposure to ambient temperature increases the likelihood of pathogen growth. There is also increased risk of cross-contamination at this step of the risk pathway.
Step 6: Consumer cooking behaviours. In 33% of cases, consumers reported cooking their Qurbani medium-rare or pink in the middle (lamb chops, liver, etc). This indicates a significant difference in risk for offal, as offal is more likely to be contaminated during the slaughter process and have internal contamination unlike muscle. Medium-rare or pink in the middle meat may also present a risk, however, contamination of meat would only be present on the surface, lowering the risk to the consumer if the surface of the meat reaches the required kill time of 70 °C for 2 minutes or equivalent (uncertainty).
5.3 Risk assessment
5.3.1 Risk level for each scenario
We conclude that a difference in risk to consumers exists between the two scenarios. The risk level for the typical scenario is very low (very rare but cannot be excluded) (see Table 8: Interpretation of probability categories used in this risk assessment. Table from ACMSF (ACM/1065) adapted from EFSA 2006 modified from OIE 2004.). The risk level for the worst-case scenario is low (rare but does occur).
The longest period of transportation by consumers from the slaughterhouse to the home was around two hours. Under the reasonably-foreseeable worst-case scenario defined above we therefore assume that meat and offal may remain at temperatures as high as 30°C for up to four hours following slaughter; a longer time period between slaughter and collection is likely to mean a lower carcase temperature at the time of collection as a result of longer chilling time at the slaughterhouse. Taking into account the growth characteristics of Salmonella (Section 3.1.1) and STEC (Section 3.1.3), we estimate that populations of both pathogens may increase by 1-2 log10 CFU/g under these conditions. Vegetative cells of C. perfringens are unlikely to increase significantly enough between the two scenarios to pose a higher level of risk, even in the worst-case scenario, given the high dose necessary for infection, if starting levels are low.
5.3.2 Risk level for each scenario when compared to meat and offal supplied in line with regulation
In the typical scenario observed, there is not a significant difference in the microbiological health risk to the final consumer associated with the supply of Qurbani meat and offal.
If the requirement to fully chill offal is not followed, if the meat and offal are exposed to increased temperature abuse (for example in unrefrigerated vehicles) and are undercooked or left marinading for a long time at room temperature, as per the worst-case scenario, there is a significant difference in the microbiological health risk to the final consumer.
We believe the worst-case scenario will occur less frequently, based on the data collected showing risky behaviours are observed in the minority. The risk can also be reduced if consumer hygiene practices are good, and meat/offal is thoroughly cooked as reported in 67% of cases. This is additionally supported by the epidemiological data, in terms of very low numbers of outbreaks connected to Eid al-Adha.
Thorough cooking by the consumer is likely to effectively mitigate the direct increase in risk when consuming meat or offal that has not undergone thorough chilling before leaving the slaughterhouse. However, the potential for an increase to consumer risk via cross-contamination during preparation still exists (uncertainty).
The uncertainty in this risk assessment is classed as high (interpretation provided in Table 9), primarily due to the limited number of data sources available for several key parameters and the fact that data are reliant on self-reporting by FBOs, OVs and consumers. The uncertainties identified as most important for this assessment are listed in Section 5.4.
Table 8: Interpretation of probability categories used in this risk assessment. Table from ACMSF (ACM/1065) adapted from EFSA 2006 modified from OIE 2004.
| Probability category | Interpretation |
|---|---|
| Negligible | So rare that it does not merit to be considered |
| Very low | Very rare but cannot be excluded |
| Low | Rare, but does occur |
| Medium | Occurs regularly |
| High | Occurs very often |
| Very high | Events occur almost certainly |
Table 9: Qualitative categories for expressing uncertainty in relation to qualitative risk estimates. Table from ACMSF (ACM/1065), adapted from EFSA 2006.
| Uncertainty category | Interpretation |
|---|---|
| Low | There are solid and complete data available; strong evidence is provided in multiple references; authors report similar conclusions |
| Medium | There are some but no complete data available; evidence is provided in a small number of references; authors report conclusions that vary from one another |
| High | There are scarce or no data available; evidence is not provided in references but rather in unpublished reports or based on observations, or personal communication; authors report conclusions that vary considerably between them. |
5.4 Uncertainties
Questions aimed at FBOs/OVs:
A larger sample of:
- the average core/surface temperature achieved for ovine offal
- the average core/surface temperature achieved for bovine offal
- the average core/surface temperature achieved for caprine offal
- the average core/surface temperature achieved for sheep/lambs
- the average core/surface temperature achieved for cattle
- the average core/surface temperature achieved for goats
- reasons for UIN/IN status
- time between slaughter and collection
Questions aimed at consumers:
- the temperature of carcase/offal when it arrives at consumer home, and the length of the journey there (if not transported under refrigerated conditions).
- how many carcases/offal are being collected by individual consumers?
- length of time carcase/offal remains at room temperature upon arrival at consumer home
- what does portioning meat at home entail? Do some consumers butcher whole/half carcases in the home?
For future questionnaires, multiple choice questions would provide more useful data for data analysis than free text responses. Further amendments to the questions in the questionnaires are suggested in the Appendix, Section 7.5.
Other uncertainties:
- recent prevalence and enumeration of Salmonella spp., C. perfringens and STEC in beef, lamb and goat meat and red offal within the UK, post slaughter.
- the difference in contamination levels between meat and offal, between animals from different farm types and between products from premises with no audit actions, IN and UIN.
- whether or not contaminating strains of Salmonella, C. perfringens and STEC would behave similarly to strains used in lab-based studies of growth on meat and when compared to Combase modelling.
- epidemiological data linking cases of illness to the consumption of Qurbani meat/offal
- do butchers further chill meat before it reaches final consumers? (and if so details of the process)
6. References
- Abdelrahim, A, Radomski, N, Delannoy, S, Djellal, S, Le Négrate, M, Hadjab, K, Fach, P, Michel-Yves Mistou, J and Firmesse, O. Frontiers | Large-Scale Genomic Analyses and Toxinotyping of Clostridium perfringens Implicated in Foodborne Outbreaks in France | Microbiology [WWW Document], n.d. URL https://www.frontiersin.org/articles/10.3389/fmicb.2019.00777/full?utm_… (accessed 1.25.22).
- Abdullah, S., Sharkas, G., Sabri, N., Iblan, I., Abdallat, M., Jriesat, S., Hijawi, B., Khanfar, R., Al Nsour, M., 2013. Mass gathering in Aqaba, Jordan, during Eid Al Adha, 2010. East Mediterr Health J 19, 29–33. https://doi.org/10.26719/2013.19.Supp2.S29
- AHBD 2021 EID11 Scholars opinion on fully chilled offal (002).pdf, n.d.
- AHDB 2020 Qurbani-leaflet, n.d.
- AHDB 2021 EID01 QOP Qurbani supply to final consumer.pdf, n.d.
- An epidemiological review of gastrointestinal outbreaks associated with Clostridium perfringens, North East of England, 2012–2014 | Epidemiology & Infection | Cambridge Core, n.d.
- BARANYI, J., TAMPLIN, M.L., 2004. ComBase: A Common Database on Microbial Responses to Food Environments†. Journal of Food Protection 67, 1967–1971. https://doi.org/10.4315/0362-028X-67.9.1967
- Barnes, E.M., Despaul, J.E., Ingram, M., 1963. The Behaviour of a Food Poisoning Strain of Clostridium welchii in Beef. Journal of Applied Bacteriology 26, 415–427. https://doi.org/10.1111/j.1365-2672.1963.tb04792.x
- Biglia, A., Gemmell, A., Foster, H., Evans, J., 2017. Temperature and energy performance of domestic cold appliances in households in England. International Journal of Refrigeration 85C, 543–555. https://doi.org/10.1016/j.ijrefrig.2017.10.022
- Brynestad, S., Granum, P.E., 2002. Clostridium perfringens and foodborne infections. Int J Food Microbiol 74, 195–202. https://doi.org/10.1016/s0168-1605(01)00680-8
- Bucur, F.I., Grigore-Gurgu, L., Crauwels, P., Riedel, C.U., Nicolau, A.I., 2018. Resistance of Listeria monocytogenes to Stress Conditions Encountered in Food and Food Processing Environments. Frontiers in Microbiology 9, 2700. https://doi.org/10.3389/fmicb.2018.02700
- Cartwright, E.J., Jackson, K.A., Johnson, S.D., Graves, L.M., Silk, B.J., Mahon, B.E., 2013. Listeriosis Outbreaks and Associated Food Vehicles, United States, 1998–2008. Emerg Infect Dis 19, 1–9. https://doi.org/10.3201/eid1901.120393
- Conserve Energy Future - Advantages and Disadvantages of Intensive Farming [WWW Document], n.d. URL https://www.conserve-energy-future.com/advantages-disadvantages-intensi… (accessed 6.3.21).
- Daniel, N., Casadevall, N., Sun, P., Sugden, D., Aldin, V., 2018. The Burden of Foodborne Disease in the UK 2018 95.
- de Jong, A.E.I., Rombouts, F.M., Beumer, R.R., 2004. Behavior of Clostridium perfringens at low temperatures. International Journal of Food Microbiology 97, 71–80. https://doi.org/10.1016/j.ijfoodmicro.2004.03.030
- DEFRA, 2015. Halal and kosher slaughter [WWW Document]. GOV.UK. URL https://www.gov.uk/guidance/halal-and-kosher-slaughter (accessed 6.8.21).
- DEFRA 2021 United Kingdom Food Security Report 2021: Theme 5: Food Safety and Consumer Confidence - GOV.UK [WWW Document], n.d. URL https://www.gov.uk/government/statistics/united-kingdom-food-security-r… (accessed 1.24.22).
- Desai, A.N., Anyoha, A., Madoff, L.C., Lassmann, B., 2019. Changing epidemiology of Listeria monocytogenes outbreaks, sporadic cases, and recalls globally: A review of ProMED reports from 1996 to 2018. Int J Infect Dis 84, 48–53. https://doi.org/10.1016/j.ijid.2019.04.021
- Dolan, G, Foster, K, Lawler, J, Amar, C, Swift, C, Aird, H and Gorton, R. 2015 An epidemiological review of gastrointestinal outbreaks associated with Clostridium perfringens, North East of England, 2012–2014 | Epidemiology & Infection | Cambridge Core [WWW Document], n.d. URL https://www.cambridge.org/core/journals/epidemiology-and-infection/arti… (accessed 1.26.22).
- Duncan, C.L., Strong, D.H., 1968. Improved Medium for Sporulation of Clostridium perfringens. Applied Microbiology. https://doi.org/10.1128/am.16.1.82-89.1968
- EFSA 2013 Scientific Opinion on the public health hazards to be covered by inspection of meat from sheep and goats, n.d. . EFSA Journal. https://doi.org/10.2903/j.efsa.2013.3265
- EFSA 2014 Scientific Opinion on the public health risks related to the maintenance of the cold chain during storage and transport of meat. Part 1 (meat of domestic ungulates) | EFSA [WWW Document], n.d. URL https://www.efsa.europa.eu/en/efsajournal/pub/3601 (accessed 12.10.21).
- EFSA, 2017. Zoonosis Monitoring. Trends and sources of zoonosis and zoonotic agents in foodstuffs, animals and feedingstuffs.
- EFSA, 2019. Zoonosis Monitoring. Trends and sources of zoonosis and zoonotic agents in foodstuffs, animals and feedingstuffs.
- EFSA and ECDC Dec 2021. The European Union One Health 2020 Zoonoses Report | EFSA [WWW Document], n.d. URL https://www.efsa.europa.eu/en/efsajournal/pub/6971 (accessed 1.28.22).
- Eikmeier, D., Medus, C., Smith, K., 2018. Incubation period for outbreak-associated, non-typhoidal salmonellosis cases, Minnesota, 2000–2015. Epidemiology & Infection 146, 423–429. https://doi.org/10.1017/S0950268818000079
- EFSA 2018. Listeria monocytogenes contamination of ready-to-eat foods and the risk for human health in the EU | EFSA [WWW Document]. URL https://www.efsa.europa.eu/en/efsajournal/pub/5134 (accessed 11.16.21).
- EFSA and ECDC 2021. The European Union One Health 2019 Zoonoses Report. EFS2 19. https://doi.org/10.2903/j.efsa.2021.6406
- EFSA and ECDC, 2019. The European Union One Health 2018 Zoonoses Report. EFS2 17. https://doi.org/10.2903/j.efsa.2019.5926
- European Food Safety Authority and European Centre for Disease Prevention and Control (EFSA and ECDC), 2019. EFSA and ECDC 2019. The European Union One Health 2018 Zoonoses Report. EFS2 17. https://doi.org/10.2903/j.efsa.2019.5926
- The EFSA Journal, 2005. Opinion of the Scientific Panel on biological hazards (BIOHAZ) related to Clostridium spp in foodstuffs. EFS2 3. https://doi.org/10.2903/j.efsa.2005.199
- Evans, E.W., Redmond, E.C., 2016. Time-Temperature Profiling of United Kingdom Consumers’ Domestic Refrigerators. Journal of Food Protection 79, 2119–2127. https://doi.org/10.4315/0362-028X.JFP-16-270
- Farming inspections [WWW Document], n.d. . GOV.UK. URL https://www.gov.uk/government/collections/farming-inspections (accessed 6.30.21).
- Field Vet Lead, Personal Communication. Jan 2022. UIN/IN status of slaughterhouses.
- Fredriksson-Ahomaa, M., Stolle, A., Korkeala, H., 2006. Molecular epidemiology of Yersinia enterocolitica infections. FEMS Immunol Med Microbiol 47, 315–329. https://doi.org/10.1111/j.1574-695x.2006.00095.x
- FSA, 2020. Food chain information [WWW Document]. Food Standards Agency. URL https://www.food.gov.uk/business-guidance/food-chain-information (accessed 11.5.21).
- Food Standards Agency, 2010. A UK wide survey of microbiological contamination of fresh red meats on retail sale. B18018.
- García, S., Heredia, N., 2011. Clostridium perfringens: A Dynamic Foodborne Pathogen. Food Bioprocess Technol 4, 624–630. https://doi.org/10.1007/s11947-009-0182-2
- Gaulin, C., Ramsay, D., Dion, R., Simard, M., Gariépy, C., Levac, É., Hammond-Collins, K., Michaud-Dumont, M., Gignac, M., Fiset, M., 2018. Veal Liver as Food Vehicle for Human Campylobacter Infections. Emerg Infect Dis 24, 1130–1133. https://doi.org/10.3201/eid2406.171900
- Glynn, J.R., Bradley, D.J., 1992. The relationship between infecting dose and severity of disease in reported outbreaks of Salmonella infections. Epidemiol Infect 109, 371–388. https://doi.org/10.1017/s0950268800050366
- Golden, N.J., Crouch, E.A., Latimer, H., Kadry, A.-R., Kause, J., 2009. Risk assessment for Clostridium perfringens in ready-to-eat and partially cooked meat and poultry products. J Food Prot 72, 1376–1384. https://doi.org/10.4315/0362-028x-72.7.1376
- Gormley, F.J., Little, C.L., Rawal, N., Gillespie, I.A., Lebaigue, S., Adak, G.K., 2011. A 17-year review of foodborne outbreaks: describing the continuing decline in England and Wales (1992–2008). Epidemiology & Infection 139, 688–699. https://doi.org/10.1017/S0950268810001858
- Grau, F.H., 1983. Growth of Escherichia coli and Salmonella typhimurium on Beef Tissue at 25°C. Journal of Food Science 48, 1700–1704. https://doi.org/10.1111/j.1365-2621.1983.tb05064.x
- Hanna, M.O., Smith, G.C., Savell, J.W., McKEITH, F.K., Vanderzant, C., 1982. Microbial Flora of Livers, Kidneys and Hearts from Beef, Pork and Lamb: Effects of Refrigeration, Freezing and Thawing. J Food Prot 45, 63–73. https://doi.org/10.4315/0362-028x-45.1.63
- Hess, I.M.R., Neville, L.M., McCarthy, R., Shadbolt, C.T., McAnulty, J.M., 2008. A Salmonella Typhimurium 197 outbreak linked to the consumption of lambs’ liver in Sydney, NSW. Epidemiol Infect 136, 461–467. https://doi.org/10.1017/S0950268807008813
- Holland, D., Thomson, L., Mahmoudzadeh, N., Khaled, A., 2020. Estimating deaths from foodborne disease in the UK for 11 key pathogens. BMJ Open Gastroenterology 7, e000377. https://doi.org/10.1136/bmjgast-2020-000377
- Im, M.C., Seo, K.W., Bae, D.H., Lee, Y.J., 2016. Bacterial Quality and Prevalence of Foodborne Pathogens in Edible Offal from Slaughterhouses in Korea. J Food Prot 79, 163–168. https://doi.org/10.4315/0362-028X.JFP-15-251
- Khan, M., Nazir, J., Anjum, A.A., Ahmad, M.-U.-D., Nawaz, M., Shabbir, M.Z., 2015. Toxinotyping and antimicrobial susceptibility of enterotoxigenic Clostridium perfringens isolates from mutton, beef and chicken meat. J Food Sci Technol 52, 5323–5328. https://doi.org/10.1007/s13197-014-1584-3
- Kothary, M.H., Babu, U.S., 2001. Infective Dose of Foodborne Pathogens in Volunteers: A Review. Journal of Food Safety 21, 49–68. https://doi.org/10.1111/j.1745-4565.2001.tb00307.x
- Kwaasi, A.A.A., 2003. MICROBIOLOGY | Classification of Microorganisms, in: Caballero, B. (Ed.), Encyclopedia of Food Sciences and Nutrition (Second Edition). Academic Press, Oxford, pp. 3877–3885. https://doi.org/10.1016/B0-12-227055-X/00773-2
- Li, J., McClane, B.A., 2006. Further Comparison of Temperature Effects on Growth and Survival of Clostridium perfringens Type A Isolates Carrying a Chromosomal or Plasmid-Borne Enterotoxin Gene. Appl Environ Microbiol 72, 4561–4568. https://doi.org/10.1128/AEM.00177-06
- Little, C.L., Richardson, J.F., Owen, R.J., de Pinna, E., Threlfall, E.J., 2008. Campylobacter and Salmonella in raw red meats in the United Kingdom: Prevalence, characterization and antimicrobial resistance pattern, 2003–2005. Food Microbiology 25, 538–543. https://doi.org/10.1016/j.fm.2008.01.001
- Williams, M, Personal Communication Nov 2021. Offal contamination
- Mackey, B.M., Roberts, T.A., Mansfield, J., Farkas, G., 1980. Growth of Salmonella on chilled meat. J Hyg (Lond) 85, 115–124. https://doi.org/10.1017/s0022172400027121
- McPhail, N, Dykes, G, Eustace I, 2005. Investigation of microbiological growth on offal during cooling. Meat and livestock Australia.
- NISRA, 2011. statistics [WWW Document]. URL https://www.ninis2.nisra.gov.uk/public/SearchResults.aspx?sk=QS*&AllAny… (accessed 11.12.21).
- Phetxumphou, K., 2016. Shiga Toxin-producing E. coli O157:H7 Dose-Response Estimation from Outbreak Data. Presented at the IAFP 2016 Annual Meeting, Iafp.
- Rahman, A., Bonny, T.S., Stonsaovapak, S., Ananchaipattana, C., 2011. Yersinia enterocolitica: Epidemiological Studies and Outbreaks. Journal of Pathogens 2011, e239391. https://doi.org/10.4061/2011/239391
- Roberts, T.A., 1968. Heat and Radiation Resistance and Activation of Spores of Clostridium welchii. Journal of Applied Bacteriology 31, 133–144. https://doi.org/10.1111/j.1365-2672.1968.tb00350.x
- Smith, S., Schaffner, D.W., 2004. Evaluation of a Clostridium perfringens Predictive Model, Developed under Isothermal Conditions in Broth, To Predict Growth in Ground Beef during Cooling. Applied and Environmental Microbiology. https://doi.org/10.1128/AEM.70.5.2728-2733.2004
- Stubbington, P. Personal Communication Dec 2021. Audit status, n.d.
- Stubbington, P. Personal Communication. Dec 2021. Qurbani donations, n.d.
- Talukdar, P.K., Udompijitkul, P., Hossain, A., Sarker, M.R., 2016. Inactivation Strategies for Clostridium perfringens Spores and Vegetative Cells. Appl Environ Microbiol 83, e02731-16. https://doi.org/10.1128/AEM.02731-16
- Taormina, P.J., Dorsa, W.J., 2004. Growth Potential of Clostridium perfringens during Cooling of Cooked Meats. Journal of Food Protection 67, 1537–1547. https://doi.org/10.4315/0362-028X-67.7.1537
- Teunis, P.F.M., Kasuga, F., Fazil, A., Ogden, I.D., Rotariu, O., Strachan, N.J.C., 2010. Dose–response modeling of Salmonella using outbreak data. International Journal of Food Microbiology 144, 243–249. https://doi.org/10.1016/j.ijfoodmicro.2010.09.026
- The Behaviour of a Food Poisoning Strain of Clostridium welchii in Beef | Request PDF, n.d. . ResearchGate.
- Tomkin, B and Swift-Eckrich A, 2015. The Significance of time-temperature to growth of foodborne pathogens_during refrigeration at 40-50°F. Presented during the Joint FSIS/FDA Conference on_Time/Temperature. November 18, Washington, DC
- Whitworth, 2021. Salmonella outbreak affected 20 in Wales [WWW Document]. Food Safety News. URL https://www.foodsafetynews.com/2021/11/salmonella-outbreak-affected-20-… (accessed 2.8.22).
- World Health Organisation, 2018. Shiga toxin producing Escherichia coli (STEC) and food: attribution, caharacterisation and monitoring. Microbiological Risk Assessment Series 31.
- Willardsen, R, Busta, F, Allen C and Smith L 1978. Growth and survival of Clostridium perfringens during constantly rising temperatures - Journal of Food Science - Wiley Online Library [WWW Document], n.d. URL https://ift.onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2621.1978.tb… (accessed 1.25.22).
- Williams, M, Personal Communication, Dec 2021. Active Refrigeration.
- Wilson, D., Dolan, G., Aird, H., Sorrell, S., Dallman, T.J., Jenkins, C., Robertson, L., Gorton, R., 2018. Farm-to-fork investigation of an outbreak of Shiga toxin-producing Escherichia coli O157. Microb Genom 4, e000160. https://doi.org/10.1099/mgen.0.000160
- World Atlas. Best Countries for Animal Welfare [WWW Document], n.d. URL https://www.worldatlas.com/articles/best-countries-for-animal-welfare.h… (accessed 6.15.21).
- World Health Organization, Nations, F. and A.O. of the U., 2002. Risk assessments of Salmonella in eggs and broiler chickens. World Health Organization.
- Zschöck, M., Hamann, H.P., Kloppert, B., Wolter, W., 2000. Shiga-toxin-producing Escherichia coli in faeces of healthy dairy cows, sheep and goats: prevalence and virulence properties. Lett Appl Microbiol 31, 203–208. https://doi.org/10.1046/j.1365-2672.2000.00789.x
7. Appendix
7.1 Mitigations for providing Qurbani meat and offal
Further details on the mitigations that were in place in 2021 are given below.
For carcase meat, partial chilling of meat before direct supply (meat to be placed under active refrigeration for at least 30 minutes before dispatch). Active refrigeration is defined as chilling using set parameters to control the temperature, for example thermostatic control within a chiller, in comparison to refrigeration where the temperature cannot be controlled and monitored, such as a refrigerated cool box. Parameters used are unknown and may be dependent on the FBO’s Hazard Analysis and Critical Control Points system but it is expected that the temperature is set to at least the legislative chilling requirement as a minimum (Pers comms., Williams, M., Dec 2021).
For carcase meat, supply of health information and consumer advice on the cooking and handling of the Qurbani meat (AHDB 2020). This includes:
- keeping transport times to a minimum
- Once home cut it up and do one of the following 3 things:
1. Chill it – put it in the coldest part of the fridge (should be below 5°C)
2. Freeze it
3. Cook it – make sure meat is well cooked throughout
- no information is provided on shelf life of the product
- measures in place to minimise cross-contamination, including suitable wrapping
The following mitigations have been proposed by industry*:
- demonstration of suitable microbiological sampling and testing results and/or hygiene history. Supply of Qurbani will only be permitted in slaughterhouses that are:
A. conducting routine microbiological testing of carcases in line with the required frequency that applies to their throughput (this applies to all slaughterhouses, there is no additional requirement for those supplying Qurbani), and
B: have had satisfactory results for the previous two months (satisfactory is determined by OVs), and
C: following all latest audits were not placed in the Improvement Necessary/Urgent Improvement Necessary categories (this was in place during 2020, but not for 2021. Inclusion of this mitigation for future years is under discussion). This is further discussed in Section 3.4.3.
Evidence of the mitigations proposed by industry is lacking, therefore, this risk assessment DOES NOT consider these mitigations to be in place and concludes an overall risk from slaughterhouses within UIN, IN and no improvements needed categories.
For offal:
- partial chilling of offal (carcase and offal to be placed under active refrigeration for at least 30 minutes before dispatch)
- additional consumer information provided about the risks specific to offal and the Scholars opinion in relation to providing fully chilled offal from the previous day’s production. Islamic Scholars are Muslims trained in Islam and Islamic law. The Scholars opinion as stated by the Agriculture and Horticulture Development Board (AHDB), agreed that since the legal procedure is in place to protect the consumer from increased microbiological risks associated with handling and consuming of un-chilled offal, the following measures can be taken (EID11, 2021):
1. Consumers collecting their meat or carcases from their agent on the first day of Qurbani (10th of Dhul Hijja) may be offered chilled non-Qurbani offal from previous slaughter or they could return at a later time or date to collect fully chilled Qurbani offal
2. Consumers collecting their carcases/meat from their agent on the second and third days (11th and 12th of Dhul Hijja) may be offered Qurbani offal from the previous day’s slaughter.
- consumers provided with strengthened advice about handling, storage and cooking, including advice that the offal must be consumed within 24 hours.
- during Qurbani 2021 the mitigations listed above (partial chilling of offal, additional consumer information and strengthened advice on handling, storage and cooking) was limited to those consumers collecting offal (not chilled in line with the regulatory requirements) directly from the slaughterhouse who traditionally expected their specific offal with their Qurbani carcase (expected to be 5-10% of those visiting). In all other cases, for example, when collected by butchers or agents, the offal had to be fully chilled in accordance with legislative requirements (3°C core temp). It is currently uncertain whether some, all, or no consumers will have the option of collecting offal not chilled in accordance with the regulatory requirements in future years.
7.2 Pubmed literature search
The following search terms were used in Pubmed:
(Qurbani OR Eid al-Adha) AND (Outbreak OR foodborne illness OR foodborne disease OR illness OR disease) NOT (COVID-19 OR Covid OR Emerging infectious diseases OR Emerging infectious disease OR early infant diagnosis)
15 results were returned, of which 3 were considered relevant based on title and abstract screening and are discussed in further detail in the text.
7.3 Slaughterhouse audits
Slaughterhouses undergo periodic audits carried out by OVs and depending on their performance may be assessed as “Urgent Improvement Necessary” (UIN) or “Improvement Necessary” (IN). The audit covers (Pers. comms., Stubbington, P. Dec 2021):
- controls in place to minimise potential spread of animal diseases
- animal welfare standards
- controls ensuring hygienic production
- environmental hygiene and food hygienic practices
- effectiveness of food safety systems based on the principles of Hazard analysis and Critical Control Points
- handling of animal by-products and waste
- effectiveness of controls and removal of specified risk material from cattle, sheep and goats.
Not all sections need to be completed for every establishment. This depends on the type of establishment and the activities it carries out.
FBOs are placed in either category (UIN or IN) based on the number of major non-compliances, or, if applicable critical non-compliances:
- IN: 3-6 major non-compliances during audit period and no critical non-compliance
- UIN: 1 critical or >6 major non-compliances during audit period
Non-compliances are defined as:
- Major: Likely to compromise public health (including food safety), animal health and welfare or may lead to the production and handling of unsafe or unsuitable food if no remedial action is taken.
- Critical: the contravention poses an imminent and serious risk to public health (including food safety), animal health and welfare.
It is important to note that the mitigation that slaughterhouses placed under UIN or IN status would not supply Qurbani was proposed by industry and was in place for Qurbani 2020. This mitigation was not in place for Qurbani 2021 therefore slaughterhouses assigned UIN or IN status following audit were able to supply Qurbani meat and offal. Whether or not this mitigation will be in place for future years is under discussion.
This risk assessment DOES NOT consider this mitigation to be in place and concludes an overall risk from slaughterhouses within UIN, IN and no improvements needed categories.
7.4 Temperature achieved post-slaughter
Data collected from the 2021 FBO survey showed a total of 27,326 carcases were supplied marginally chilled. Based on the responses from the questionnaire, it can be assumed that meat supplied via agents such as butchers will normally undergo further chilling, such as in a refrigerated van, before delivery to final consumers (uncertainty). A smaller number of carcases, 10,173, were supplied fully chilled in 2021, based on FBO responses.
A breakdown of the average number of carcases that were supplied fully and marginally chilled directly to the consumer is summarised in Table 10. Of the 17 FBOs who provided a response, 5 FBOs or 29% of respondents supplied carcases (of all species) that were fully chilled directly to the consumer. 10 FBOs, or 59% of respondents supplied marginally chilled sheep/lamb carcases directly to the consumer. 3 FBOs, or 18% of respondents supplied marginally chilled ‘other species’ carcases directly to the consumer. 2 of the FBOs indicated these were cattle but the remaining FBO did not state the species supplied.
Table 10: Summary of the temperature of the carcase as reported by FBOs providing carcases directly to consumers in 2021.
| FBOs supplied | Fully chilled: all species | Marginally chilled: Sheep/lamb | Marginally chilled: Other species |
|---|---|---|---|
| Number of FBOs that supplied | 5 | 10 | 3 |
| Average number of carcases | 508 (33 - 1768) | 687 (8 - 3000) | 9 (1 - 23) |
| Number of FBOs that did not supply | 12 | 7 | 13 |
| No response/unknown | 3 | 3 | 4 |
When the FBOs were asked how many carcases were supplied fully and marginally chilled to the consumer via butchers/wholesalers, most similarly responded that these had been provided marginally chilled. These data are summarised in Table 11. Six FBOs, or 44% of respondents supplied some carcases (of all species) that were fully chilled to consumers via butchers/wholesalers and 9, or 56% of respondents, did not. 12 FBOs, or 86% of respondents, supplied marginally chilled sheep/lamb carcases to consumers via butchers/wholesalers, although only 10 specified how many carcases they supplied. 2 FBOs did not supply marginally chilled sheep/lamb. Five FBOs, or 36% or respondents, supplied marginally chilled ‘other species’ carcases to consumers via butchers/wholesalers, and 10 did not.
Table 11: summary of the temperature of the carcase as reported by FBOs providing carcases to consumers via butchers or wholesalers in 2021. * This average was calculated using values provided from 10 FBOs.
| FBOs supplied | Fully chilled: all species | Marginally chilled: Sheep/lamb | Marginally chilled: Other species |
|---|---|---|---|
| Number of FBOs supplying | 6 | 12 | 5 |
| Average number of carcases | 1342 (range 96 - 4000) | 2025 (range 150 - 4629)* | 35 (range 5 - 64) |
| Number of FBOs that did not supply | 9 | 2 | 10 |
| No response/unknown | 4 | 3 | 4 |
The OVs were asked a similar question in the 2021 questionnaire and the results suggest that most Qurbani meat was marginally chilled. 19 slaughterhouses provided ‘marginally chilled’ meat, 9 provided ‘partially chilled’ meat and 6 provided ‘chilled’ meat only. Of those that did provide marginally or partially chilled meat, it is unclear what proportion was provided as such, and what proportion was provided as chilled, as the respondents were not asked (uncertainty).
7.5 Suggestions for future questionnaires
Some suggestions for future questions in consumer questionnaire to further bridge evidence gaps and reduce uncertainty:
- how many carcases does each consumer collect?
- do consumers who collect directly from the slaughterhouse butcher their own whole/half carcase or take to a butcher?
Questions that can be amended/removed in future questionnaires:
Consumer questionnaire:
- was the Qurbani is collected in any sort of refrigerated storage such as a cool box or cool bag (for those who answered yes for agent/appointee/butcher)
- what is the time it takes between collection and getting the Qurbani home (for those who answered yes for agent/appointee/butcher)
- what do you do with your Qurbani when it arrives home? (the question should be reformulated to better understand how long the Qurbani stays at room temperature upon arrival)
OV questionnaire:
- did customers signed customer declarations? (reworded to make it more precise)
- were customers provided with customer information leaflets (reworded to make it more precise)
- was Qurbani offal supplied chilled? (N.B All offal supplied via butchers/wholesalers acting as agents) should have been chilled in accordance with the legal requirements) – reword to make more neutral
FBO questionnaire:
- where do you source your Qurbani animals from? (make multiple choice)
- what is your average daily throughput outside of the Qurbani period? (make multiple choice)
- what was your total throughput on DAY 1 of Qurbani? (make multiple choice)
- was the throughout larger on DAY 1 of Qurbani compared to an average day?
- what is the total number of LAMB and SHEEP Qurbani that were supplied over the WHOLE Qurbani period? (make multiple choice)
- what was the number of carcases supplied directly to consumer (wording it as the number of carcases/offal supplied overall and then what proportion was supplied to consumer and to wholesalers/butchers)
- what was the number of consumers that also picked up offal/pluck with their carcase, or on its own, rather than weight of offal
Annexes
England and Wales
Hanes diwygio
Cyhoeddwyd: 10 Mehefin 2022
Diweddarwyd ddiwethaf: 12 Medi 2023